Tachycardia
Content is incomplete and may be incorrect. |
Introduction
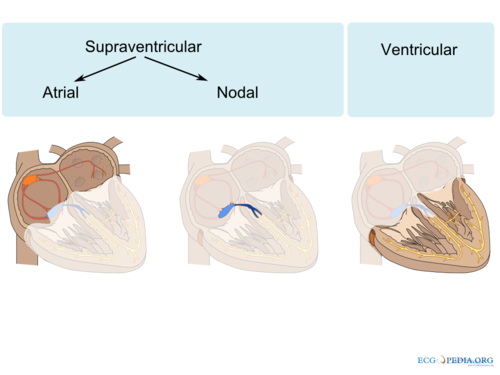
Differentiation between supraventricular tachycardias (SVT) and ventricular tachycardias (VT) can be challenging, especially in acute emergency settings. SVT's are rhythm disturbances in the atria or AV-nodal ring or rhythm disorders in which these structures are involved. VT's are rhythm disorders that only involve the ventricles. It can both take place in the myocardial tissue and the conduction system tissue.
Supra-ventricular tachycardia
Atrial arrhythmias
The following arrhyhmias arise in the atrium. Dependent on the amount of conduction block in the AV-node the ventricles follow the atrial contraction. However, at higher atrial rates the AV-node starts to block conduction from atrium to ventricle.
Sinus Tachycardia
Pathophysiology:
When the sinus node fires with a frequency between 100-180bpm, the term sinustachycardia is used. The maximum heart rate a person can achieve during exercise can be calculated by subtracting the age in years from 210. Usually it is a physiological reaction to stress (exercise, inflammation, stress). External factors can increase the heart rate like coffee and alcohol or drugs. The term inappropriate sinus tachycardia is used when the sinus node has a exaggerated response to stress.
Clinical diagnosis:
A sinus tachycardia usually has a gradual start and ending. Diagnosis on the ECG can be made by the morphology of the P-wave. The P-wave has the same morphology during sinus tachycardia as during normal sinus rhythm.
Management:
No treatment is indicated, usually the sinustachycardia will pass when the external trigger is removed. If patients have complaints a beta-blocker can be administered.
Atrial Tachycardia
Pathophysiology:
Atrial tachycardia is a tachycardia resulting from fast firing in an ectopic focus in the atria. It has a frequency of above the 100bpm. In some patients the tachycardia has multiple foci. This results in different P-wave morphologies on the ECG. The result of firing can be due to all mechanisms of arrhythmias and is dependent on the causes of the atrial tachycardia.
Clinical diagnosis:
Atrial tachycardias have a wide clinical presentation. Complaints of palpitation and a fast regular heart rate are common. On the ECG an atrial tachycardia can be detected through the P-wave morphology. The P-wave has an other morpholgy depending on the foci of the atrial tachycardia. A ECG in resting condition can help distinguish different morphologies. When administrating adenosine the AV-conduction blocks and firing from the atrium continues, thereby clearly identifying the atrial source of the tachycardia.
Management:
Atrial tachycardias can be treated with anti-arrhythmic medication, for instance with beta-blockers. If medication does not help, catheter ablation might locate the arrhythmia and ablate the source of repeated firing.
Atrial Flutter
Pathophysiology:
Atrial flutter is a type of atrial tachycardia that is dependent of the cavotricuspid isthmus. The isthmus between the caval vein and tricuspid is an area of slow conduction. Due to this slow conduction re-entry around the tricuspid annulus can exist. This re-entry produces a typical arrhythmia with activates the atria at a certain frequency. If the re-entry circuit moves counterclockwise a typical atrial flutter is produced. If the re-entry circuit moves clockwise, a atypical flutter is seen. The causes and risk are comparable with atrial fibrillation.
Clinical diagnosis:
An atrial flutter can be detected on the ECG by it typical sawtooth pattern and atrial frequency. An atrial flutter has a frequency of 300 bpm, which conducts to the ventricles in 2:1, 3:1 or 4:1 manner. The P-wave morphology has a sawtooth like appearance and in a typical flutter has a negative vecter in the inferior leads. The first part of the P-wave is fast, the second path slow. In a atypical flutter the inferior leads have a positive vector.
Management:
A patient with an atrial flutter requires cardioversion. This can be achieved with anti-arrhythmic drugs or electrical cardioversion. Patients with atrial flutter require anti-coagulation as in atrial fibrillation according to the CHADSVASc score. Atrial flutters are amendable to catheter ablation. This is a very succesfull procedure, with few complications in the hands of an experiences electrophysiologist.
Atrial Fibrillation
Pathophysiology:
The pathophysiology of atrial fibrillation is complex and incompletely understood. In atrial fibrillation there is chaotic depolarisation with multiple foci, that spin around each other. In most patients the trigger of atrial fibrillation results from extra beats in from the pulmonary veins. This is due to myocardial sleeves growing into the pulmonary veins, which are triggered to fire extra beats due a variaty of modulators (e.i. the autonomic nerve system). These triggers can trigger the atria into forming multiple self-perpetuating re-entry circuits. The ability of the atria to sustain atrial fibrillation is dependable on atrial structural changes (fibrosis). Due to this fast and rapid activation of the atria, there is no functional mechanical activity left. This results in the most feared complication of atrial fibrillation, namely forming of blood clots (with for instance stroke as a result). The atrial standstill does not effectively pump blood to the ventricle, and blood can coagulate in for instance the left atrial appendage. The strokes resulting from atrial fibrillation are often more severe than other causes of stroke.
Clinical diagnosis:
Atrial fibrillation is the most common supraventricular arrhythmia in Western society. It is characterized by the absence of clear P-waves on the surface ECG and an irregular ventricular ventricular rate. On physical examination an irregular pulse can be felt, however this is not diagnostic of atrial fibrillation as other causes can cause an irregular pulse (atrial or ventricular extra systoles). The cardiac output is reduced due to lack of atrial kick. Furthermore due to the higher ventricular rate the heart has not enough time to completely fill with blood. Atrial fibrillation is classified according to the clinical presentation of atrial fibrillation:
- Paroxysmal atrial fibrillation: Episodes atrial fibrillation lasting shorter than 7 days and terminating spontaneously
- Persistent atrial fibrillation: Episodes of atrial fibrillation not terminating spontaneously or lasting longer than 7 days
- Long standing persistent atrial fibrillation: Persistent atrial fibrillation for more than one year.
- Permanent atrial fibrillation: Accepted atrial fibrillation, no strategies of rhythm control are pursued.
Management:
Atrial fibrillation can be managed with anti-arrhythmic medication or more invasive treatment strategies. Studies have shown no benefit of rhyhtm control over rate control, thus the selection of strategy is mainly dependent of patient and atrial fibrillation characteristics. Independent of the treatment strategy, proper anti-coagulation is important and necessary in patients with risk factors.
- Rate control: In atrial fibrillation the ventricle can have a fast irregular rate that can be difficult to tolerate by a patient. On of the strategies in managing atrial fibrillation is to control ventricular rate <120bpm. In this strategy no attempt is made to achieve sinus rhythm. This is the only treatment option in patients with permanent atrial fibrillation. Due to the fast irregular ventricular rate a dilated tachycardiomyopathy can develop and proper rate control can revert these ventricular changes. Rate control can be achieved with beta-blockers, Ca-antagonist and digoxine.
- Invasive treatment:
- His-Ablation with pacemaker implantation: Patients with accepted atrial fibrillation and complaints of a fast irregular ventricular frequency who do not tolerate medication can be helped with a targeted His bundle ablation with catheter ablation to induce complete AV-block. A implanted pacemaker can take over the ventricular firing frequency independent of the atrium.
- Invasive treatment:
- Rhythm control: In rhythm control all efforts are made to achieve and maintain sinus rhythm. This can be done with anti-arrhythmic drugs. Most effective are the Class IC and III anti-arrhythmic drugs. Overall rhythm control is difficult and anti-arrhythmic drugs have many (pro-arrhythmic) side effects. Therefore prescription of these drugs should occur with caution.
- Invasive treatment:
- Catheter ablation: Medical therapy is not always sufficient to maintain sinus rhythm. In the last decade of 20th century it was discovered that atrial fibrillation is triggered from the pulmonary veins and that selective ablation of these trigger sites can reduce atrial fibrillation recurrence. As this technique evolved it is now common to ablate an area around the pulmonary veins to isolate them from the atrial tissue. The left atrium is approached through the inter-atrial septum and with the use of imaging and electrocardiographic signals a 3D map is made to navigate the atria. The pulmonary vein isolation can be performed with multiple energy sources. This is a difficult and long procedure, that depending on the technique used has (severe) complications. The success rate of the procedure varies on the experience of the operator (40-60%). Often the success rate can be increased by performing multiple procedures.
- Surgical treatment: Surgery is a more invasive, but more effective modality to treat atrial fibrillation. The classical cut and sew Maze procedure is a open chest procedure that requires extra-corporeal circulation. In this procedure the atrium is cut and sewn again to compartmentalize the atrium en therefore prevent the atrium maintaining atrial fibrillation. In recent years a less invasive procedure has developed to treat atrial fibrillation. This minimal invasive surgery is performed through thoractomy or thoracoscopy and is performed on a beating heart. A pulmonary vein isolation is performed with a clamp and if patients have persistent atrial fibrillation additional left atrial lessions are made on the atrium to compartmentalize the atrium. Finally the left atrial appendage is removed to reduce the occurrence of stroke. This procedure has a success rate of 68% after one year.
- Invasive treatment:
- Anticoagluation treatment: Proper anti-coagulation is important in patients with atrial fibrillation to reduce the occurence of stroke. In patient with atrial fibrillation the indication of anti-coagulation is based on certain risk-factors a patients has. A score is created to fascilitate this descision making. The CHADS2VASc score incorporates the following risk factors:
- C: Congestive heart failure [1 major point]
- H: Hypertension [1 major point]
- A: Age>75years [1 major point]
- D: Diabetes [1 major point]
- S: Stroke/Embolism [2 major points]
- A: Age>65years [1 minor point]
- Sc: Female Sex [1 minor point]
If a patient has 2 minor points or 1 major point anti-coagulation with coumarins is indicated. If a patient has no indication for coumarins no anti-coagulation is necessary.
AV node arrhythmias
This section covers the arrhythmias in which the AV node is critical in maintaining the arrhythmia. Most of these arrhythmias share the common characteristic that AV-node blocking or delaying manoeuvres or medication (adenosine) can terminate the arrhythmia.
AV junctional tachycardia
An AV junctional tachycardia is a tachycardia resulting from regular frequent firing (60-100 bpm) of the AV-node. It has the characteristics of a small QRS with a retrograde or no P-wave. The P-wave is not always visible because it can be hidden in the QRS complex. If it is visible it is negative in the inferior leads and narrow, suggesting an AV-nodal origin. The small QRS is not preceded by a p-wave as atrium and ventricle are activated both from the AV-node.
AV Nodal Re-entry Tachycardia (AVNRT)
Pathophysiology:
AVNRT is a regular arrhythmia relying only on the dual AV-physiology for its maintenance. The AV-node has two pathways; a fast pathway with fast conduction times and a slow pathway with exhibits slow conduction. The fast pathway has a longer refractory period than the slow pathway. Due to these characteristics re-entry formation is possible. Normally the impulse from the atria is conducted through the fast pathway to the ventricle. The impulse also travels through the slow pathway, but reaches a refractory ending of the AV-node (as the fast pathway already has conducted the impulse and activated this part of the AV-node). When an extra premature atrial contraction occurs it encounters a refractory fast-pathway (which has a longer refractory period). It enters the slow pathway and when it reaches the end of this pathway it can conduct to the (now restored) end of the AV-node to the ventricles and back into the fast pathway. The result is a ventricular activation with a retrograde P-wave. If the slow pathway is restored when the impulse reaches the end (atrial side) of the fast pathway, the impulse can re-enter the slow-pathway and a re-entry mechanism is established. This is usually the mechanism of an AVNRT and is called a typical AVNRT and is found in 90% of the patient with an AVNRT. There exists two other form of AVNRT that take a different route through the AV-node. Firstly there is an atypical AVNRT in which the impulse travels through the fast pathway and returns through the slow pathway. The result of this AVNRT is a retrograde P-wave which appears far from the QRS complex. Finally there is a rare AVNRT which in patients with two slow pathways. The impulse enters en re-enters through a slow pathway.
Clinical diagnosis:
It is a fast regular small complex tachycardia with a frequency of 180-250 bpm. It is more common in female than in men (3:1) and has a sudden onset. Palpitation can cause the Frog sign; neck vein palpitations which occur due to simultaneous contraction of the atrial and ventricle. The atria cannot empty in the ventricles and therefore expulse their content in the venous circulation. A typical AVNRT can be diagnosed on the ECG by a RP distance of 100ms. The P wave is hidden in the QRS complex or appears directly after the QRS complex. An atypical AVNRT has a retrograde P appearing far away from the QRS, as it has to travel through the slow pathway. A registration of the onset can often be quite helpful in establishing the diagnosis AVNRT.
Management:
Termination is possible by vagal manoeuvres (blowing on the wrist, carotid sinus massage) or medication (adenosine, verapamil, diltiazem). If manoeuvres or medication fails electrocardioversion can be performed.
AV Nodal Re-entry Tachycardia (AVNRT)
Pathophysiology:
AVRT are tachycardias with a re-entry circuit compromising the entire heart. Atria, AV-node, ventricle and an extra bundle are an essential part of this circuit. The pre-requisite of an AVRT is the existence of an extra bundle between the atria and ventricle. This bundle can bypass the AV-node. The following bundles exist:
- Bundle of Kent: A connection between atria and ventricles most often located on the lateral side of the atria\ventricles.
- Lown-Ganong-Levine bundle: A connection between the atria and the bundle of His, effectively bypassing the AV-node.
- Maheim-Bundle: A connection between AV conduction system and ventricles with AV-like conduction properties.
Depending on the conduction characteristics of the bundle and the direction of conduction two different AVRT circuits can manifest:
- Orthodrome AV re-entry tachycardia: The impulse travels through the normal conduction system and returns to the atria via the accessory bundle.
- Antidrome AV re-entry tachycardia: The impulse travels antrograde through the accessory bundle and activates the ventricles. The impulse returns through the normal conduction system to the atria.
Clinical diagnosis:
- Orthodrome AV re-entry tachycardia: There is a P-wave (other morphology than sinus rhythm) followed by small QRS-complex
- Antidrome AV re-entry tachycardia: The tachycardia resembles a broad-complex tachycardia and is follow by a retrograde P-wave originating from the AV-node.
Management:
Anti-arrhythmic drugs or ablation
Ventricular tachycardia
Ventricular tachycardias (VT's) are rhythm disturbances that arise in the ventricles.
History
Symptoms can arise in every ventricular tachycardia, depending on the heart rate, the presence of underlying heart disease and the degree of systolic and diastolic heart failure. Various symptoms are:
- Palpitations
- Abnormal chest sensation
- Dyspnea
- Angina
- Presyncope (lightheadedness, weakness, diaphoresis)
- Syncope
- Cardiogenic shock
Additional information about drug use is mandatory. Toxic levels of digoxin and cocain can lead to VT's. Also additional information about family history of sudden cardiac death is helpfull, as it is a strong predictor of susceptibility to ventricular arrhythmias and sudden cardiac death.
Physical Examination
Although the diagnosis of VT is generally made by a 12 lead ECG, the following physical symptoms may be present:
- Cannon "A" waves on the jugular venous pulse in the neck. These represent intermittant retrograde propulsion of blood into the jugular veins during right atrial contraction against a closed AV valve. This is evidence of AV dissociation.
- Decreased or variable amplitude of the carotid or peripheral pulses. This is related to the intermittent periods of atrial and ventricular synchronization, which transiently augment cardiac output.
- Variable intensity of the first heart sound (although this is difficult with a rapid heart rate).
- Variable splitting of the first and second heart sounds, and intermittent presence of a third and/or fourth heart sound.
Diagnostic Evaluation
- Exercise testing: Exercise testing is recommended in adult patients with ventricular tachycardias who have an intermediate or greater probability of having coronary heart disease by age, gender and symptoms. It is meant to provoke ischemic changes or ventricular arrhythmias.
- Ambulatory (Holter) ECG: Ambulatory ECG is necessary if the diagnosis needs to be clarified, by detecting arrhythmias, QT-interval changes, T-wave alternans (TWA) or ST-segment changes.
- Echocardiography, Cardiac CT, MRI: Echocardiography is recommended in patients with ventricular tachycardias who are suspected of having a structural heart disease. If echocardiography does not provide accurate assessment of the left and right ventricular function and/or structural changes, cardiac CT or MRI can be done.
- Exercise testing with an image modality (echocardiography or nuclear perfusion): Some patients with ventricular arrhythmias have an intermediate probability of coronairy heart disease, but their ECG is less reliabe (because of digoxin use, LVH, greater than 1mm ST-segment depression at rest, WPW syndrome or LBBB). For detecting silent ischemia in these patients exercise testing with an image modality can be done. If patients are unable to perform exercise, a pharmacological stress test with an imaging modality can be done.
- Coronary angiography: Coronary angiography can diagnose or exclude the presence of significant obstructive coronairy heart disease in patients with ventricular arrhythmias who have an intermediate or greater probability of having coronairy heart disease.
- Electrophysiological testing: Electrophysiological testing can be performed to guide and assess the efficacy of VT ablation in patients with ventricular arrhythmias. It can also be done to clarify the mechanism of broad complex tachycardias in patients with coronairy heart disease.
Overview of ventricular tachycardias
(figure: overview of ventricular tachycardias)
Ventricular tachycardia
Ventricular tachycardia (VT) is defined as a sequence of three or more ventricular beats. The frequency is often 110-250 bpm. Ventricular tachycardias often origin around old scar tissue in the heart, e.g. after myocardial infarction. Also electrolyte disturbances and ischemia can cause ventricular tachycardias. The cardiac output is often strongly reduced during VT resulting in hypotension and loss of conciousness. VT is a medical emergency as it can deteriorate into ventricular fibrillation and thus mechanical cardiac arrest.
Definitions
- Non-sustained VT: three or more ventricular beats with a maximal duration of 30 seconds.
- Sustained VT: a VT of more than 30 seconds duration (or less if treated by electrocardioversion within 30 seconds).
- Monomorphic VT: all ventricular beats have the same configuration.
- Polymorphic VT: the ventricular beats have a changing configuration. The heart rate is 100-333 bpm.
- Biphasic VT: a ventricular tachycardia with a QRS complex that alternates from beat to beat. Associated with digoxin intoxication and long QT syndrome.
Localisation of the origin of a ventricular tachycardia
Determination of the location (or exit site) where a ventricular tachycardia originated, can be helpful in understanding the cause of the VT and is very helpful when planning an ablation procedure to treat a ventricular tachycardia. (new page for localization)
Differential diagnosis
(Non)sustained VT may be idiopathic, but occurs most frequently in patients with underlying structural heart disease of various types including:
- Coronary heart disease (CHD) with prior myocardial infarction (is the most frequent cause in developed countries)
- Hypertrophic cardiomyopathy
- Dilated cardiomyopathy
- Mitral valve prolapse
- Aortic stenosis
- Complex congenital heart disease
- Cardiac sarcoidosis
- Arrhythmogenic RV cardiomyopathy/dysplasia
Treatment
Hemodynamical instability:
- Electrocardioversion
Haemodynamical stability in a regular monomorphic broadcomplex tachycardia (systolic blood pressure >100 mmHg):
- Pharmacological treatment can be considered with Procaïnamide or Amiodaron
Ventricular flutter
Ventricular flutter is a ventricular tachycardia that occurs at a very rapid rate (often around 300 bpm), mostly caused by re-entry. The QRS complexes are regular and usually monomorphic and show a typical sinusoidal pattern. During ventricular flutter the ventricles depolarize in a circular pattern, which prevents good function. Most often this results in a minimal cardiac output and subsequent ischemia. Often deteriorates into ventricular fibrillation.
Treatment
Electrocardioversion is the only treatment for ventricular flutter.
Ventricular fibrillation
Ventricular fibrillation (VF) is identified by the complete absence of properly formed QRS complexes and no obvious P waves. Instead of uniform activation of the ventricular myocardium, there are uncoördinated series of very rapid, ineffective contractions of the ventricle caused by many chaotic electrical impulses. In recent onset VF the QRS complexes are of high amplitude at rates greater than 320 bpm, which manifest random changes in morphology, width and height. It appears as a completely chaotic rhythm. If VF continues, the fibrillatory waves become fine and can resemble asystole in these cases.
Treatment
VF is lethal if the patient is not treated immediately. It gives rise to a mechanical standstill of the heart, because the heart is not able to pump normally anymore. Electrocardioversion is the only treatment for ventricular fibrillation.
Accelerated idio-ventricular rhythm
Accelerated idioventricular rhythm (AIVR) is a relatively benign form of ventricular tachycardia. It is (mostly) a regular repetitive ventricular rhythm rate around 60-120 bpm, but mostly 80-100. It is the result of an enhanced ectopic ventricular rhythm, which is faster than normal intrinsic ventricular escape rhythm (<40 bpm), but slower than ventricular tachycardia (over 100-120 bpm). It often occurs during reperfusion after a myocardial infarction. AIVR is not predictive marker for early VF; however, recent debate has started whether among patients with successfull coronary intervention, AIVR is a sign of ventricular dysfunction and therefore a slightly worde prognosis. AIVR can also occur in infants. By this definition, this is a ventricular rhythm of no more than 20% faster than the sinus rate and occuring in the absence of other heart disease. This arrhythmia typically resolves spontaneously during the first months of life (in contrast to an infant with incessant VT which can be due to discrete myocardial tumors or congenital cardiomyopathy).
Treatment
AIVR is generally a transient, self-limiting rhythm and resolves as sinus rate surpasses the rate of AIVR. It rarely causes hemodynamic instability and rarely requires treatment.
Torsades de Pointes
Torsades de pointes (TdP) is a ventricular tachycardia associated with a prolonged QTc interval on the resting ECG. It is on the ECG characterized by twisting of the peaks of the QRS complexes around the isoelectric line during the arrhythmia (changing axis). Torsade de pointes is typically initiated by a short-long-short interval. A ventricle extrasystole (first beat: short) is followed by a compensatory pause. The following beat (second beat: long) has a longer QT interval. If the next beat follows shortly thereafter, there is a good chance that this third beat falls within the QT interval, resulting in the R on T phenomenon and subsequent Torsades de pointes.
Differential diagnosis
- Aquired long QT syndrome (drugs causing long QT syndrome: http://www.azcert.org/medical-pros/drug-lists/drug-lists.cfm)
- Congenital long QT syndrome
Treatment
Electrocardioversion is the first treatment for TdP.
Additional treatments are:
- Withdrawal of any offending drugs and correction of electrolyte abnormalities (potassium repletion up to 4.5 to 5 mmol/liter).
- Acute and long-term cardiac pacing in patients with TdP presenting with heart block, symptomatic bradycardia or recurrent pause-dependent TdP
- Intravenous magnesium sulfate for patients with QT prolongation and few episodes of TdP.
- Beta blockers combined with cardiac pacing as acute therapy for patients with TdP and sinus bradycardia.
- Isoproterenol as temporary treatment in patients with recurrent pause-dependent TdP who do not have congenital long QT syndrome.
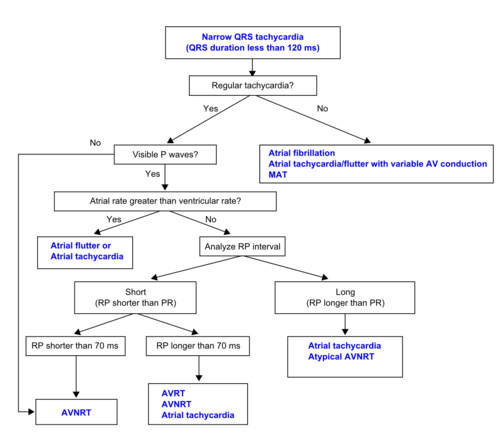
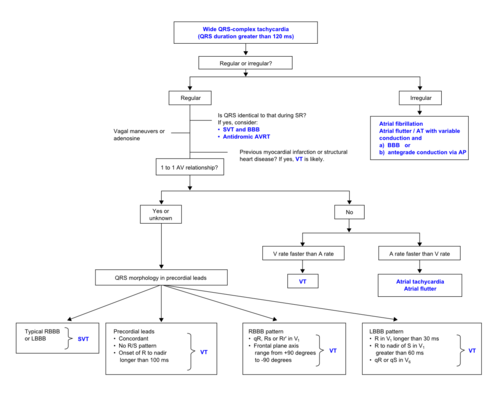
Differentiation between SVT and VT
To differentiate between supraventricular tachycardias and ventricular tachycardias a 12 lead ECG is the cornerstone of the diagnostic process. At first, the physician has to make a differentiation between a small or broad complex tachycardia.
Definitions
Small complex tachycardia:
- QRS duration < 120 ms.
- A small complex tachycardia is most likely to be a SVT. However, also a septal VT or His-tachycardia can appear as a small complex tachycardia.
Broad complex tachycardia:
- QRS duration > 120 ms.
- A broad complex tachycardia can be due to a SVT with aberration, pre-exited tachycardia (eg antidrome re-entry tachycardia) or VT.
Differentiation
Treatment
Haemodynamical instability (systolic blood pressure less than 100 mmHg):
- electrical cardioversion
Haemodynamical stability in a regular small complex tachycardia:
- Carotid massage (after palpation and ausculatation of carotid arteries for exclusion of carotid occlusion/stenosis)
- Vasalva manoevre
- Adenosine bolus (if patient is not asthmatic or having COPD)
- Verapamil (if patient is not having systolic heart failure)
- Beta-blocker (if patient is not having systolic heart failure)
References
- ESC Textbook of Cardiovascular Medicine, 2nd Edition
- ECGpedia.org