Ventricular tachycardia: Difference between revisions
No edit summary |
No edit summary |
||
| Line 5: | Line 5: | ||
===History=== | ===History=== | ||
Symptoms can arise in every ventricular tachycardia, depending on the heart rate, the presence of underlying heart disease and the degree of systolic and diastolic heart failure. | Symptoms can arise in every ventricular tachycardia, depending on the heart rate, the presence of underlying heart disease and the degree of systolic and diastolic heart failure. Various symptoms are: | ||
*Palpitations | *Palpitations | ||
*Abnormal chest sensation | *Abnormal chest sensation | ||
| Line 16: | Line 14: | ||
*Cardiogenic shock | *Cardiogenic shock | ||
Additional information about drug use is mandatory. Toxic levels of digoxin and cocain can lead to VT's. Also additional information about family history of sudden cardiac death is helpfull, as it is a strong predictor of susceptibility to ventricular arrhythmias and sudden cardiac death. | |||
===Physical Examination=== | ===Physical Examination=== | ||
Although the diagnosis of VT is generally made by a 12 lead ECG, the following physical symptoms may be present: | Although the diagnosis of VT is generally made by a 12 lead ECG, the following physical symptoms may be present: | ||
*Decreased or variable amplitude of the carotid or peripheral pulses. This is related to the intermittent periods of atrial and ventricular synchronization, which transiently augment cardiac output. | *Decreased or variable amplitude of the carotid or peripheral pulses. This is related to the intermittent periods of atrial and ventricular synchronization, which transiently augment cardiac output. | ||
*Cannon | *Cannon "A" waves on the jugular venous pulse in the neck. These represent intermittant retrograde propulsion of blood into the jugular veins during right atrial contraction against a closed AV valve. This is evidence of AV dissociation. | ||
*Variable intensity of the first heart sound (although this is difficult with a rapid heart rate). | *Variable intensity of the first heart sound (although this is difficult with a rapid heart rate). | ||
*Variable splitting of the first and second heart sounds, and intermittent presence of a third and/or fourth heart sound. | *Variable splitting of the first and second heart sounds, and intermittent presence of a third and/or fourth heart sound. | ||
===Diagnostic Evaluation=== | ===Diagnostic Evaluation=== | ||
*'''Exercise testing:''' Exercise testing is recommended in adult patients with ventricular tachycardias who | *'''Exercise testing:''' Exercise testing is recommended in adult patients with ventricular tachycardias who have an intermediate or greater probability of having coronary heart disease by age, gender and symptoms. It is meant to provoke ischemic changes or ventricular arrhythmias. | ||
*'''Ambulatory (Holter) ECG:''' Ambulatory ECG is necessary if the diagnosis needs to be clarified, by detecting arrhythmias, QT-interval changes, T-wave alternans (TWA) or ST-segment changes. | *'''Ambulatory (Holter) ECG:''' Ambulatory ECG is necessary if the diagnosis needs to be clarified, by detecting arrhythmias, QT-interval changes, T-wave alternans (TWA) or ST-segment changes. | ||
*'''Echocardiography, Cardiac CT, MRI:''' Echocardiography is recommended in patients with ventricular tachycardias who are suspected of having structural heart disease. If echocardiography does not provide accurate assessment of the left and right ventricular function and/or structural changes, cardiac CT or MRI can be done. | *'''Echocardiography, Cardiac CT, MRI:''' Echocardiography is recommended in patients with ventricular tachycardias who are suspected of having a structural heart disease. If echocardiography does not provide accurate assessment of the left and right ventricular function and/or structural changes, cardiac CT or MRI can be done. | ||
*'''Exercise testing with an image modality (echocardiography or nuclear perfusion):''' Some patients with ventricular arrhythmias have an intermediate probability of coronary heart disease, but their ECG is less reliable (because of digoxin use, LVH, greater than 1mm ST-segment depression at rest, WPW syndrome or LBBB). For detecting silent ischemia in these patients exercise testing with an image modality can be done. If patients are unable to perform exercise, a pharmacological stress test with an imaging modality can be done. | *'''Exercise testing with an image modality (echocardiography or nuclear perfusion):''' Some patients with ventricular arrhythmias have an intermediate probability of coronary heart disease, but their ECG is less reliable (because of digoxin use, LVH, greater than 1mm ST-segment depression at rest, WPW syndrome or LBBB). For detecting silent ischemia in these patients exercise testing with an image modality can be done. If patients are unable to perform exercise, a pharmacological stress test with an imaging modality can be done. | ||
*'''Coronary angiography:''' Coronary angiography can diagnose or exclude the presence of significant obstructive coronary heart disease in patients with ventricular arrhythmias who have an intermediate or greater probability of having coronary heart disease. | *'''Coronary angiography:''' Coronary angiography can diagnose or exclude the presence of significant obstructive coronary heart disease in patients with ventricular arrhythmias who have an intermediate or greater probability of having coronary heart disease. | ||
*'''Electrophysiological testing:''' Electrophysiological testing can be performed to guide and assess the efficacy of VT ablation in patients with ventricular arrhythmias. It can also be done to clarify the mechanism of broad complex tachycardias in patients with coronary heart disease. | *'''Electrophysiological testing:''' Electrophysiological testing can be performed to guide and assess the efficacy of VT ablation in patients with ventricular arrhythmias. It can also be done to clarify the mechanism of broad complex tachycardias in patients with coronary heart disease. | ||
==Overview of ventricular tachycardias== | ==Overview of ventricular tachycardias== | ||
{| class="wikitable" font-size="90%" | {| class="wikitable" font-size="90%" | ||
Revision as of 20:37, 25 March 2013
Ventricular tachycardia
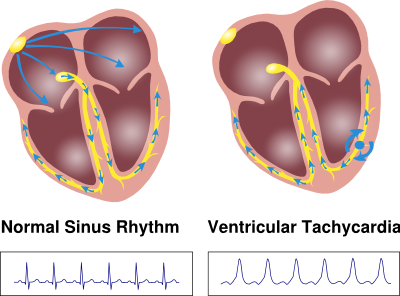
Ventricular tachycardias (VT's) are rhythm disturbances that arise in the ventricles.
History
Symptoms can arise in every ventricular tachycardia, depending on the heart rate, the presence of underlying heart disease and the degree of systolic and diastolic heart failure. Various symptoms are:
- Palpitations
- Abnormal chest sensation
- Dyspnea
- Angina
- Presyncope (lightheadedness, weakness, diaphoresis)
- Syncope
- Cardiogenic shock
Additional information about drug use is mandatory. Toxic levels of digoxin and cocain can lead to VT's. Also additional information about family history of sudden cardiac death is helpfull, as it is a strong predictor of susceptibility to ventricular arrhythmias and sudden cardiac death.
Physical Examination
Although the diagnosis of VT is generally made by a 12 lead ECG, the following physical symptoms may be present:
- Decreased or variable amplitude of the carotid or peripheral pulses. This is related to the intermittent periods of atrial and ventricular synchronization, which transiently augment cardiac output.
- Cannon "A" waves on the jugular venous pulse in the neck. These represent intermittant retrograde propulsion of blood into the jugular veins during right atrial contraction against a closed AV valve. This is evidence of AV dissociation.
- Variable intensity of the first heart sound (although this is difficult with a rapid heart rate).
- Variable splitting of the first and second heart sounds, and intermittent presence of a third and/or fourth heart sound.
Diagnostic Evaluation
- Exercise testing: Exercise testing is recommended in adult patients with ventricular tachycardias who have an intermediate or greater probability of having coronary heart disease by age, gender and symptoms. It is meant to provoke ischemic changes or ventricular arrhythmias.
- Ambulatory (Holter) ECG: Ambulatory ECG is necessary if the diagnosis needs to be clarified, by detecting arrhythmias, QT-interval changes, T-wave alternans (TWA) or ST-segment changes.
- Echocardiography, Cardiac CT, MRI: Echocardiography is recommended in patients with ventricular tachycardias who are suspected of having a structural heart disease. If echocardiography does not provide accurate assessment of the left and right ventricular function and/or structural changes, cardiac CT or MRI can be done.
- Exercise testing with an image modality (echocardiography or nuclear perfusion): Some patients with ventricular arrhythmias have an intermediate probability of coronary heart disease, but their ECG is less reliable (because of digoxin use, LVH, greater than 1mm ST-segment depression at rest, WPW syndrome or LBBB). For detecting silent ischemia in these patients exercise testing with an image modality can be done. If patients are unable to perform exercise, a pharmacological stress test with an imaging modality can be done.
- Coronary angiography: Coronary angiography can diagnose or exclude the presence of significant obstructive coronary heart disease in patients with ventricular arrhythmias who have an intermediate or greater probability of having coronary heart disease.
- Electrophysiological testing: Electrophysiological testing can be performed to guide and assess the efficacy of VT ablation in patients with ventricular arrhythmias. It can also be done to clarify the mechanism of broad complex tachycardias in patients with coronary heart disease.
Overview of ventricular tachycardias
| example | regularity | atrial frequency | ventricular frequency | origin (SVT/VT) | p-wave | effect of adenosine | |
|---|---|---|---|---|---|---|---|
| Wide complex (QRS>0.12) | |||||||
| Ventricular Tachycardia | File:Vt small.svg | regular (mostly) | 60-100 bpm | 110-250 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) |
| Ventricular Fibrillation | File:Vf small.svg | irregular | 60-100 bpm | 400-600 bpm | ventricle (VT) | AV-dissociation | none |
| Ventricular Flutter | File:Vflutt small.svg | regular | 60-100 bpm | 150-300 bpm | ventricle (VT) | AV-dissociation | none |
| Accelerated Idioventricular Rhythm | File:Aivr small.svg | regular (mostly) | 60-100 bpm | 50-110 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) |
| Torsade de Pointes | File:Tdp small.svg | regular | 150-300 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) | |
| Bundle-branch re-entrant tachycardia* | regular | 60-100 bpm | 150-300 bpm | ventricles (VT) | AV-dissociation | no rate reduction | |
| * Bundle-branch re-entrant tachycardia is extremely rare | |||||||
Ventricular tachycardia
Ventricular tachycardia (VT) is defined as a sequence of three or more ventricular beats. The rate is often 110-250 bpm. Ventricular tachycardias often origin around old scar tissue in the heart, e.g. after myocardial infarction. Also electrolyte disturbances and ischemia can cause ventricular tachycardias. The cardiac output is often strongly reduced during VT resulting in hypotension and loss of consciousness. VT is a medical emergency as it can deteriorate into ventricular fibrillation and thus mechanical cardiac arrest.
Definitions
- Non-sustained VT: Three or more ventricular beats with a maximal duration of 30 seconds.
- Sustained VT: A VT of more than 30 seconds duration (or less if treated by electrocardioversion within 30 seconds).
- Monomorphic VT: All ventricular beats have the same configuration.
- Polymorphic VT: The ventricular beats have a changing configuration. The heart rate is 100-333 bpm.
- Biphasic VT: A ventricular tachycardia with a QRS complex that alternates from beat to beat. Associated with digoxin intoxication and long QT syndrome.
Localisation of the origin of a ventricular tachycardia
Determination of the location (or exit site) where a ventricular tachycardia originated can be helpful in understanding the cause of the VT and is very helpful when planning an ablation procedure to treat a ventricular tachycardia. The location can be determined with the QRS morphology:
- RBBB/LBBB morphology:
- RBBB: origin in the left ventricle
- LBBB: origin in the right ventricle
- Inferior/superior axis (lead II, III and aVF):
- Inferior axis (positive in lead II, III and aVF): origin superior wall
- Superior axis (negative in lead II, III and aVF): origin inferior wall
- Basal/apical (lead V5-V6):
- Positive concordance in V5-6: basal origin
- Negative concordance in V5-6: apical origin
Differential diagnosis
(Non)sustained VT may be idiopathic, but occurs most frequently in patients with underlying structural heart disease of various types including:
- Coronary heart disease (CHD) with prior myocardial infarction (is the most frequent cause in developed countries)
- Hypertrophic cardiomyopathy
- Dilated cardiomyopathy
- Mitral valve prolapse
- Aortic stenosis
- Complex congenital heart disease
- Cardiac sarcoidosis
- Arrhythmogenic RV cardiomyopathy/dysplasia
Treatment
Hemodynamical instability:
- Electrocardioversion
Haemodynamical stability in a regular monomorphic broadcomplex tachycardia (systolic blood pressure >100 mmHg):
- Pharmacological treatment can be considered with Procaïnamide or Amiodaron
Ventricular flutter
Ventricular flutter is a ventricular tachycardia that occurs at a very rapid rate (often around 300 bpm) and results from re-entry. The QRS complexes are regular and usually monomorphic and show a typical sinusoidal pattern. During ventricular flutter the ventricles depolarize in a circular pattern at a high rate, which prevents good function. Most often this results in a minimal cardiac output and subsequent ischemia. Often deteriorates into ventricular fibrillation.
Treatment
Electrocardioversion is the only treatment for ventricular flutter.
Ventricular fibrillation
Ventricular fibrillation (VF) is identified by the complete absence of properly formed QRS complexes. Instead of uniform activation of the ventricular myocardium, there are uncoördinated series of very rapid, ineffective contractions of the ventricle caused by many chaotic electrical impulses. In recent onset VF the electrical activity is of higher amplitude at rates greater than 320 bpm, which manifest random changes in morphology, width and height. It appears as a completely chaotic rhythm. If VF continues, the fibrillatory waves become fine and can resemble asystole in these cases.
Treatment
VF is lethal if the patient is not treated immediately. It gives rise to a mechanical standstill of the heart, because there is no pump function. Electrocardioversion is the only treatment for ventricular fibrillation.
Accelerated idio-ventricular rhythm
Accelerated idioventricular rhythm (AIVR) is a relatively benign form of ventricular tachycardia. It is (mostly) a regular repetitive ventricular rhythm rate around 60-120 bpm, but mostly 80-100. It is the result of an enhanced ectopic ventricular rhythm, which is faster than normal intrinsic ventricular escape rhythm (<40 bpm), but slower than ventricular tachycardia (over 100-120 bpm). It often occurs during reperfusion after a myocardial infarction. AIVR is not a predictive marker for early VF; however, recent debate has started whether among patients with successful coronary intervention, AIVR is a sign of ventricular dysfunction and therefore a slightly worse prognosis. AIVR can also occur in infants. By definition, AIVR is a ventricular rhythm of no more than 20% faster than the sinus rate and occuring in the absence of other heart disease. This arrhythmia typically resolves spontaneously during the first months of life (in contrast to an infant with incessant VT which can be due to discrete myocardial tumors or congenital cardiomyopathy).
Treatment
AIVR is generally a transient, self-limiting rhythm and resolves as sinus rate surpasses the rate of AIVR. It rarely causes hemodynamic instability and rarely requires treatment.
Torsades de Pointes
Torsades de pointes (TdP) is a ventricular tachycardia associated with a prolonged QTc interval on the resting ECG. The ECG during TdP is characterized by twisting of the peaks of the QRS complexes around the isoelectric line during the arrhythmia (changing axis). Torsade de pointes is typically initiated by a short-long-short interval. A ventricle extrasystole (first beat: short) is followed by a compensatory pause. The following beat (second beat: long) has a longer QT interval. If the next beat follows shortly thereafter (third beat: short), there is a good chance that this third beat falls within the QT interval, resulting in the R on T phenomenon and subsequent Torsades de pointes.
See the chapter on LQTS for a list of medication and genes that can cause QT prolongation and TdP.
Treatment
Electrocardioversion is the first treatment for an unconcious patient with incessant TdP.
Additional treatments are:
- Withdrawal of any offending drugs and correction of electrolyte abnormalities (potassium repletion up to 4.5 to 5 mmol/liter, the goal should be to make the patient slightly hyperkalemic).
- Acute and long-term cardiac pacing in patients with TdP presenting with heart block, symptomatic bradycardia or recurrent pause-dependent TdP
- Intravenous magnesium sulfate can be helpful to cardiovert TdP in the acute phase in patients with few TdP episodes. If recurrence occurs a continues infusion may be beneficial.
- Beta blockers combined with cardiac pacing as acute therapy for patients with TdP and sinus bradycardia. This prevents extrasystoles and thereby short-long-short sequences.
- Isoproterenol as temporary treatment in patients with recurrent pause-dependent TdP who do not have congenital long QT syndrome.
Differentiation between SVT and VT
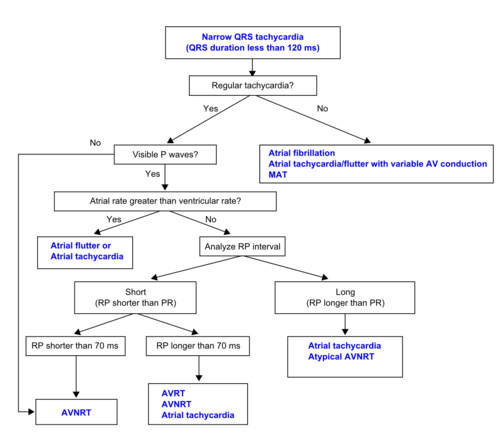
To differentiate between supraventricular tachycardias and ventricular tachycardias a 12 lead ECG is the cornerstone of the diagnostic process. At first, the physician has to make a differentiation between a small or broad complex tachycardia.
Definitions
- Narrow complex tachycardia: QRS duration < 120 ms.
A narrow complex tachycardia is most likely to be a SVT. However, also a septal VT or His-tachycardia can appear as a narrow complex tachycardia.
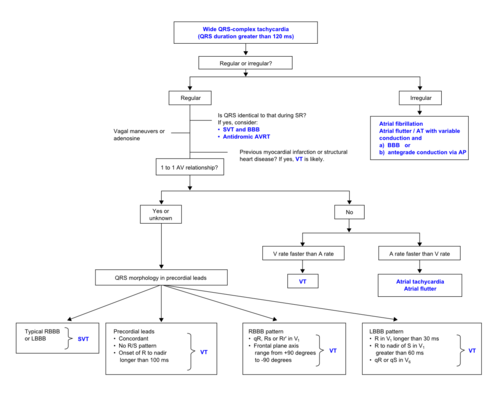
- Wide complex tachycardia: QRS duration > 120 ms.
A wide complex tachycardia can be due to a SVT with aberration, pre-exited tachycardia (eg antidrome re-entry tachycardia) or VT.
Differentiation
These are the flow charts of a small and wide complex tachycardia to differentiate between the different rhythms:
Treatment
- Haemodynamical instable (systolic blood pressure less than 100 mmHg):
- Electrical cardioversion (with anesthesia when concious)
- Haemodynamically stable regular narrow complex tachycardia:
- Carotid massage (after palpation and ausculatation of carotid arteries for exclusion of carotid occlusion/stenosis)
- Vasalva manoeuvre
- Adenosine bolus (if patient is not asthmatic or having COPD)
- Verapamil (if patient is not having systolic heart failure)
- Beta-blocker (if patient is not having systolic heart failure)