Cardiac Arrhythmias: Difference between revisions
| Line 29: | Line 29: | ||
==Cardiac conduction== | ==Cardiac conduction== | ||
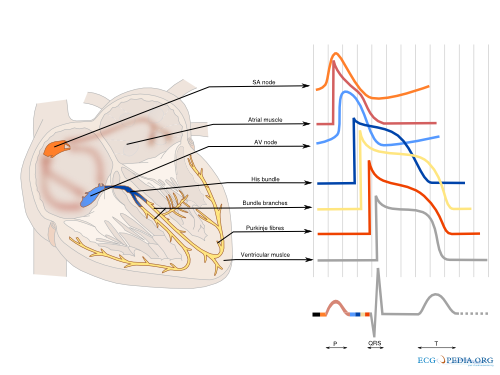
The cardiac conduction system (figure | The cardiac conduction system (figure 2) is the highway though which the electric activity of the heart spreads from the atria to the ventricles. The characteristics of the different parts of the conduction system are a result of the different characteristics of the individual myocytes. On a larger level, function is controlled predominantly by the autonomic nervous system (both vagal and sympathetic nerve system). Especially the sinus node and atrioventricular node are responsive to the autonomic nerve system. The ganglionic plexi, a conglomeration of both vagal and sympathetic nerves, form the intrinsic cardiac nerve system and innervate through a network of nerve fibers the atria and ventricles. The vagal and sympathetic nerve system are both continually active in the heart, but vagal activity dominates the tonic background stimulation of the autonomic nerve system. Moreover the heart is more susceptible to vagal stimulation. Vagal stimulation provokes a rapid response and the effect dissipates swiftly in contrast to sympathetic stimulation which has a slow onset and offset. Vagal stimulation results in a reduction in sinus node activation frequency and prolongs AV nodal conduction. These effects can occur simultaneously or independent of each other. Sympathetic stimulation exerts reverse effects, accelerating the sinus node firing frequency and improving AV nodal conduction. The autonomic nerve system has a small effect on cardiomyocytes. Vagal stimulation tends to prolong the refractory period and decrease the myocardial contractility. Sympathetic stimulation has the opposite effect on the cardiac tissue. Whereas the physiological modulation of cardiac conduction is vital to adaptation of the heart to rest and exercise the autonomic nervous system can attribute to the pathologic substrate in a diseased myocardium. | ||
[[File:Conductionsystem.svg|thumb|500px|'''Figure 2.''' The different shapes of the cardiac action potential in the heart.]] | [[File:Conductionsystem.svg|thumb|500px|'''Figure 2.''' The different shapes of the cardiac action potential in the heart.]] | ||
===Sinus node=== | ===Sinus node=== | ||
The sinus node is an densely innervated area located in the right | The sinus node is an densely innervated area located in the right atrium which is supplied by the right (55%-60%) or circumflex (40%-45%) coronary artery. It is a small structure of 10-20mm long and 2-3mm wide and contains a diversity of cells. These include pacemaker cells which are discharged synchronously due to mutual entrainment. This results in an activation wave front activating the rest of the atrium. | ||
===Atrium=== | ===Atrium=== | ||
The impulse formed in the sinus node is conducted through the atrium to the AV-node. Evidence indicates three preferential conduction pathways. The pathways show preferential conduction due to their anatomical structure and rather than specialized conduction properties. The three pathways are | The impulse formed in the sinus node is conducted through the atrium to the AV-node. Evidence indicates three preferential conduction pathways. The pathways show preferential conduction due to their anatomical structure and rather than specialized conduction properties. The three pathways are: the anterior internodal pathway, the middle internodal tract the posterior internodal pathway. The anterior internodal pathway connect to the anterior interatrial band, also known as the Bachmann bundle. This bundle of muscular tissue conducts the sinus wave front from the right to the left atrium. | ||
===AV node=== | ===AV node=== | ||
| Line 46: | Line 46: | ||
===Bundle Branches=== | ===Bundle Branches=== | ||
From the bundle of His the right bundle branch continues to the right ventricular apex. The left bundle branch splits of and divides in two or more fascicular branches. Commonly the left bundle branch consist of an anterior fascicle, | From the bundle of His the right bundle branch continues to the right ventricular apex. The left bundle branch splits of and divides in two or more fascicular branches. Commonly the left bundle branch consist of an anterior fascicle, which activates the anterosuperior portion of the left ventricle. and the thicker and more protected posterior fascicle which activates the inferoposterior part of the left ventricle. | ||
===Venticle=== | ===Venticle=== | ||
Revision as of 08:50, 28 December 2012
Sébastien Krul, MD
Content is incomplete and may be incorrect. |
General Introduction
A basic understanding of the physiological cardiac action potential and cardiac conduction system facilitates diagnosis and treatment of cardiac arrhythmias. The effects and side-effects of anti-arrhythmic drugs are depended on the influence on ion channels involved in the generation and/or perpetuation of the cardiac action potential.
Cardiac Action Potential
The cardiac action potential is a result of ions flowing through different ion channels. Ion channels are passages for ions (mainly Na+, K+, Ca2+ and Cl-) that facilitate movement through the cell membrane. Changes in the structure of these channels can open, inactivate or close these channels and thereby control the flow of ions into and out of the myocytes. Due to differences in expression of the type and structure of ion channels, the various parts of the cardiac conduction system have slightly different action potential characteristics. Ion channels are mostly a passive passageway, where movement of ions is caused by the electrochemical gradient. In addition to these passive ion channels a few active trigger-dependent channels exist that open or close in response to certain stimuli (for instance acetylcholine or ATP). These changes in the membrane potential produce and action potential lasting a few hundreds of milliseconds. Disorders in single channels can lead to arrhythmias, as seen in the section Primary_Arrhythmias. The action potential is propagated throughout the myocardium by the depolarization of the immediate environment of the cells and through intracellular coupling with gap-junctions.
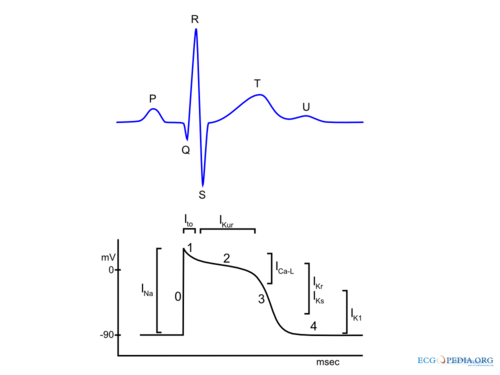
In summary during the depolarization, sodium ions (Na+) stream into the cell followed by a influx of calcium (Ca2+) ions (both from the inside (sarcoplasmatic reticulum) and outside of the cell). These Ca2+ ions cause the actual muscular contraction. Shortly thereafter potassium (K+) ions flow out of the cell, causing repolarization. During repolarization the ion concentrations return to their resting concentrations, due to the passive efflux of K+ and active exchange of Na+ with Ca2+ (Figure 1). In detail the (ventricular) action potential can be divided in five phases:
Phase 0: Rapid Depolarization
Rapid depolarization is started once the membrane potential reaches a certain threshold (about -70 to -60 mV), independent of the size of the depolarizing stimulus. This produces a rapid influx of Na+ and a rapid upstroke of the action potential. At higher potentials (-40 to -30) Ca2+ influx participates in the upstroke. In the sinus node and AV node a slower upstroke can be observed (Figure 2). This is because the upstroke in these cells is mainly mediated by the slower acting Ca2+ ion channels. The slower activation produces a slower upstroke.
Phase 1: Early Rapid Repolarization
Immediately following rapid depolarization, the inactivation of the Na+ channel (INa) and subsequent activation of the outward K+ channel (Ito) and the Na+/Ca2+ exchanger (NCX) produces a early rapid repolarization. Due to the limited role of the Na+ channel in the upstroke of sinus node and AV node cells and the subsequent slower depolarization, this rapid repolarisation is not visible in their action potentials.
Phase 2: Plateau
The plateau phase represents an equal influx and efflux of ions in or out of the cell producing a stable membrane potential. This plateau phase is predominantly observed in the ventricular action potential. The inward movement of Ca2+ through the open L-type Ca2+ channels (ICa-L) and the exchange of Na+ for internal Ca2+ by the Na+/Ca2+ exchanger (NCX) are responsible for the influx of ions during the pleateau phase. The efflux of ions is the result of outward current carried by K+ (IKur and Ks) and Cl- ions.
Phase 3: Final Rapid Repolarization
Final repolarization is mainly caused by inactivation of Ca2+ channels, reducing the influx of positive ions. Furthermore repolarizing K+ currents (delayed rectifier current IKs and IKr and inwardly rectifying current IK1 and IK,Ach) are activated which increase efflux of positive K+ ions. This results in an repolarization to the resting membrane potential.
Phase 4: Resting membrane potential
Depending on cell type the resting membrane potential is between -50 to -95 mV, sinus node and AV nodal cells have a higher resting membrane potential (-50 to -60 mV and -60 to -70 respectively) in comparison with atrial and ventricular cardiomyocytes (-80 to -90 mV). The resting membrane potential is mainly caused by differences in the the K+ outside the cell and the K+ inside the cell. Sinus node cells and AV nodal cells (and to a lesser degree Purkinje fibers cells) have a special voltage dependent channel If, the funny current. Furthermore they lack IK1, a K+ ion channel that maintains the resting membrane potential in atrial and ventricular tissue. This channel causes a slow depolarization in diastole, called the phase 4 diastolic depolarization, which results in normal automaticity. Sinus node discharges are regulated by the autonomous nerve system and due to the high firing frequency the sinus node dominates other potential pacemaker sites.
Cardiac conduction
The cardiac conduction system (figure 2) is the highway though which the electric activity of the heart spreads from the atria to the ventricles. The characteristics of the different parts of the conduction system are a result of the different characteristics of the individual myocytes. On a larger level, function is controlled predominantly by the autonomic nervous system (both vagal and sympathetic nerve system). Especially the sinus node and atrioventricular node are responsive to the autonomic nerve system. The ganglionic plexi, a conglomeration of both vagal and sympathetic nerves, form the intrinsic cardiac nerve system and innervate through a network of nerve fibers the atria and ventricles. The vagal and sympathetic nerve system are both continually active in the heart, but vagal activity dominates the tonic background stimulation of the autonomic nerve system. Moreover the heart is more susceptible to vagal stimulation. Vagal stimulation provokes a rapid response and the effect dissipates swiftly in contrast to sympathetic stimulation which has a slow onset and offset. Vagal stimulation results in a reduction in sinus node activation frequency and prolongs AV nodal conduction. These effects can occur simultaneously or independent of each other. Sympathetic stimulation exerts reverse effects, accelerating the sinus node firing frequency and improving AV nodal conduction. The autonomic nerve system has a small effect on cardiomyocytes. Vagal stimulation tends to prolong the refractory period and decrease the myocardial contractility. Sympathetic stimulation has the opposite effect on the cardiac tissue. Whereas the physiological modulation of cardiac conduction is vital to adaptation of the heart to rest and exercise the autonomic nervous system can attribute to the pathologic substrate in a diseased myocardium.
Sinus node
The sinus node is an densely innervated area located in the right atrium which is supplied by the right (55%-60%) or circumflex (40%-45%) coronary artery. It is a small structure of 10-20mm long and 2-3mm wide and contains a diversity of cells. These include pacemaker cells which are discharged synchronously due to mutual entrainment. This results in an activation wave front activating the rest of the atrium.
Atrium
The impulse formed in the sinus node is conducted through the atrium to the AV-node. Evidence indicates three preferential conduction pathways. The pathways show preferential conduction due to their anatomical structure and rather than specialized conduction properties. The three pathways are: the anterior internodal pathway, the middle internodal tract the posterior internodal pathway. The anterior internodal pathway connect to the anterior interatrial band, also known as the Bachmann bundle. This bundle of muscular tissue conducts the sinus wave front from the right to the left atrium.
AV node
The connection between atria and ventricles is facilitated through the AV node, lying in the right atrial myocardium and a penetrating part, the bundle of His. The AV node acts as a gatekeeper, regulating impulse conduction from the atrium to the ventricle. Additionally, due to the phase 4 diastolic depolarization it can exhibit impulse formation. The AV node is supplied in most cases (85%-90%) by the right coronary artery or in the remaining cases the circumflex artery.
Bundle of His
Connecting the distal AV node and the proximal bundle branches, the bundle of His is supplied by both the posterior and anterior descending coronary arteries. It is enclosed by the central fibrous body and membranous septum between the atria and the ventricles. The location and blood supply protect the bundle of His from external influences.
Bundle Branches
From the bundle of His the right bundle branch continues to the right ventricular apex. The left bundle branch splits of and divides in two or more fascicular branches. Commonly the left bundle branch consist of an anterior fascicle, which activates the anterosuperior portion of the left ventricle. and the thicker and more protected posterior fascicle which activates the inferoposterior part of the left ventricle.
Venticle
The ventricle is activated through the dense network of Purkinje fibers originating from the bundle branches. They penetrate the myocardium, but predominantly the endocardium, and are the starting point of the ventricular activation.
Mechanisms of Arrhythmia
Structural abnormalities or electric changes in the cardiomyocytes can impede impulse formation or change cardiac propagation facilitating arrhythmias. We briefly discuss the main causes of arrhythmia as these pathofysiological principles underlie to most common rhythm disorders and intervening in these mechanisms can terminate the arrhythmia.
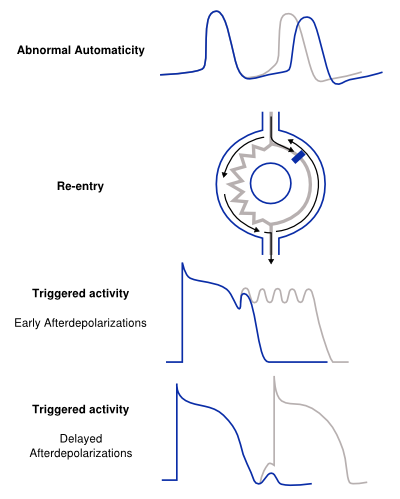
Abnormal Impulse Formation
The mechanism of abnormal automaticity is similar to the normal automaticity of sinus node cells. Abnormal automaticity can be caused by changes in the cell ion channel characteristics due to drugs or changes in the electrotonic environment. Abnormal automaticity can result from an increase of normal automaticity in non-sinus node cells or a truly abnormal automaticity in cells that don't exhibit a phase 4 diastolic depolarization.
Abnormal Automaticity
The mechanism of abnormal automaticity is similar to the normal automaticity of sinus node cells. Abnormal automaticity can be caused by changes in the cell ion channel characteristics due to drugs or changes in the electrotonic environment. Abnormal automaticity can result from an increase of normal automaticity in non-sinus node cells or a truly abnormal automaticity in cells that don't exhibit a phase 4 diastolic depolarization.
Triggered Activity
Triggered activity is activity of a cell triggered by a preceding activation. Due to early or delayed afterdepolarizations the resting membrane depolarizes and, when reaching threshold potentials, activates the cell. These afterdepolarizations are depolarizations of the membrane potential initiated by the preceding action potential. Depending on the phase of the action potential in which they arise, they are defined as early or late afterdepolarizations.
- In early afterdepolarizations depolarization occurs during the action potential (phase 2 and 3) by a diversity of causes. Early afterdepolarizations can increase duration of the repolarization phase of the action potential. This increase can create heterogeneity in refractoriness and thereby creating the substrate for a re-entry circuit (see below).
- Delayed afterdepolarizations occur after the cell has recovered after completion of repolarization. In delayed afterdepolarization an abnormal Ca2+ handling of the cell is probably responsible for the afterdepolarizations due to release of Ca2+ from the storage of Ca2+ in the sarcoplasmatic reticulum. The accumulation of Ca2+ increases membrane potential and thus depolarizes the cell when it reaches a certain threshold.
Disorders of Impulse Conduction
Conduction block or conduction delay is a frequent cause of bradyarrhythmias, however tacharrhythmias can also result from conduction block and produce a reentrant circuit. Conduction block can develop in different conditions, for instance a deceleration block or a acceleration block. These conduction block develop due to deceleration or a slow heart rate or a acceleration or fast heart rate respectively. It is important to assess the cause of conduction block as explained in the section of bradycardia, for it is important in the treatment of the conduction delay or block.
Reentry
Reentry or circus movement can arise when an area is slowly conducting thereby remaining active while the rest of the heart depolarizes. When the rest of the heart has recovered from this refractory state, and can be reactivated, the impulse in the slow conducting zone can activate the heart. This process can repeat itself and thus form the basis of a reentry tachycardia. These areas of slow conduction can be anatomical or functional or a combination of both. Examples of reentry tachycardias are atrial flutter, atrial fibrillation and ventricular tachycardias originating from an infarct zone.
References
- Braunwald's Heart Disease, 8th edition. Edited by Douglas P. Zipes. Philadelphia, Pa.: W.B. Saunders, 2008