CPVT: Difference between revisions
No edit summary |
mNo edit summary |
||
| Line 5: | Line 5: | ||
'''Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT)''' refers to a hereditary disease that is associated with exercise (or adrenergic) induced ventricular arrhythmias and/or cardiac syncope and carries an increased risk of sudden cardiac death. | '''Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT)''' refers to a hereditary disease that is associated with exercise (or adrenergic) induced ventricular arrhythmias and/or cardiac syncope and carries an increased risk of sudden cardiac death. | ||
==General features== | |||
*The diagnosis is based on adrenergic-induced bidirectional and polymorphic ventricular tachycardia. | *The diagnosis is based on adrenergic-induced bidirectional and polymorphic ventricular tachycardia. | ||
*The resting ECG is normal and the heart is structurally normal. | *The resting ECG is normal and the heart is structurally normal. | ||
| Line 13: | Line 13: | ||
*The prevalence is estimated to be 1:10.000 in Europe. | *The prevalence is estimated to be 1:10.000 in Europe. | ||
Clinical diagnosis | ==Clinical diagnosis== | ||
The clinical diagnosis of CPVT is confirmed in an individual with polymorphic VT reproducibly induced during exercise tests, isoproterenol infusion or emotion and exercise. | The clinical diagnosis of CPVT is confirmed in an individual with polymorphic VT reproducibly induced during exercise tests, isoproterenol infusion or emotion and exercise. | ||
| Line 20: | Line 20: | ||
Family members of patients with CPVT who also carry a mutation in a CPVT-associated gene are often asymptomatic. | Family members of patients with CPVT who also carry a mutation in a CPVT-associated gene are often asymptomatic. | ||
==Physical examination== | |||
Patients can present with symptoms of arrhythmias during exercise: | Patients can present with symptoms of arrhythmias during exercise: | ||
*Out-of-hospital-cardiac-arrest | *Out-of-hospital-cardiac-arrest | ||
*Syncope, pre-syncope (weakness, lightheadedness, dizziness) | *Syncope, pre-syncope (weakness, lightheadedness, dizziness) | ||
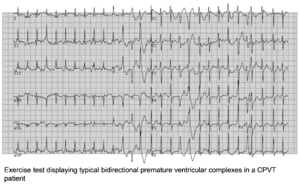
==ECG tests== | |||
[[File:Ventricular_complexes.png|thumb|300px|right]] | [[File:Ventricular_complexes.png|thumb|300px|right]] | ||
The resting ECG in CPVT is normal. However, there is a progressive ventricular ectopy as heart rate increases during exercise or isoproterenol infusion. Both the frequency and the complexity of the ventricular ectopy increase with the work load. It generally starts with monomorphic premature ventricular complexes (PVCs) and is followed bigemini and subsequently more complex arrhythmias, including doublets triplets, bidirectional ventricular tachycardia to polymorphic ventricular tachycardia. Most of the times, the arrhythmia is self-limiting. However, in some patients, especially if exercise is continued, repeated polymorphic VTs can deteriorate in ventricular fibrillation and sudden cardiac death. | The resting ECG in CPVT is normal. However, there is a progressive ventricular ectopy as heart rate increases during exercise or isoproterenol infusion. Both the frequency and the complexity of the ventricular ectopy increase with the work load. It generally starts with monomorphic premature ventricular complexes (PVCs) and is followed bigemini and subsequently more complex arrhythmias, including doublets triplets, bidirectional ventricular tachycardia to polymorphic ventricular tachycardia. Most of the times, the arrhythmia is self-limiting. However, in some patients, especially if exercise is continued, repeated polymorphic VTs can deteriorate in ventricular fibrillation and sudden cardiac death. | ||
Genetic diagnosis | |||
[[File:CPVT.jpg|thumb| | |||
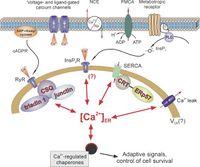
==Genetic diagnosis== | |||
[[File:CPVT.jpg|thumb|200px|left]] | |||
CPVT is caused by mutations in genes involved in the calcium homeostasis of cardiac cells. Four disease-causing genes have been identified: the ryanodine receptor 2 gene (RyR2) (60%), the cardiac calsequestrin 2 gene (CASQ2) (1-2%), the calmodulin gene (CALM1) (<1%) and the TRDM gene (<1%). Mutant RyR2 channels have a gain-of-function effect, resulting in excessive calcium release during sympathetic activation. Mutant CASQ2 causes loss of buffering capacity for calcium of the sarcoplasmatic reticulum. The mutations cause excessive calcium in the myocyte cytosol generating depolarizing membrane currents, which in turn lead to delayed afterdepolarizations and cardiac arrhythmias. | CPVT is caused by mutations in genes involved in the calcium homeostasis of cardiac cells. Four disease-causing genes have been identified: the ryanodine receptor 2 gene (RyR2) (60%), the cardiac calsequestrin 2 gene (CASQ2) (1-2%), the calmodulin gene (CALM1) (<1%) and the TRDM gene (<1%). Mutant RyR2 channels have a gain-of-function effect, resulting in excessive calcium release during sympathetic activation. Mutant CASQ2 causes loss of buffering capacity for calcium of the sarcoplasmatic reticulum. The mutations cause excessive calcium in the myocyte cytosol generating depolarizing membrane currents, which in turn lead to delayed afterdepolarizations and cardiac arrhythmias. | ||
==References== | |||
<biblio> | <biblio> | ||
#tachycardia pmid=7867192 | #tachycardia pmid=7867192 | ||
Revision as of 05:12, 22 March 2013
Auteur: Louise R.A. Olde Nordkamp
Supervisor: Arthur A.M. Wilde
Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT) refers to a hereditary disease that is associated with exercise (or adrenergic) induced ventricular arrhythmias and/or cardiac syncope and carries an increased risk of sudden cardiac death.
General features
- The diagnosis is based on adrenergic-induced bidirectional and polymorphic ventricular tachycardia.
- The resting ECG is normal and the heart is structurally normal.
- It is an inheritable cardiac arrhythmia syndrome with an autosomal dominant (RyR2) or recessive (CASQ2) inheritance.
- The arrhythmias typically occur in children and adolescents.
- The mortality rate is approximately 31% by the age of 30 years, if untreated.
- The prevalence is estimated to be 1:10.000 in Europe.
Clinical diagnosis
The clinical diagnosis of CPVT is confirmed in an individual with polymorphic VT reproducibly induced during exercise tests, isoproterenol infusion or emotion and exercise.
Patients present themselves most often with syncope or even an out-of-hospital cardiac arrest, usually during the first or second decade of life. The symptoms are always triggered by exercise or emotional stress. A family history of exercise-related syncope, seizure or sudden death is reported in 30% of the patients.
Family members of patients with CPVT who also carry a mutation in a CPVT-associated gene are often asymptomatic.
Physical examination
Patients can present with symptoms of arrhythmias during exercise:
- Out-of-hospital-cardiac-arrest
- Syncope, pre-syncope (weakness, lightheadedness, dizziness)
ECG tests
The resting ECG in CPVT is normal. However, there is a progressive ventricular ectopy as heart rate increases during exercise or isoproterenol infusion. Both the frequency and the complexity of the ventricular ectopy increase with the work load. It generally starts with monomorphic premature ventricular complexes (PVCs) and is followed bigemini and subsequently more complex arrhythmias, including doublets triplets, bidirectional ventricular tachycardia to polymorphic ventricular tachycardia. Most of the times, the arrhythmia is self-limiting. However, in some patients, especially if exercise is continued, repeated polymorphic VTs can deteriorate in ventricular fibrillation and sudden cardiac death.
Genetic diagnosis
CPVT is caused by mutations in genes involved in the calcium homeostasis of cardiac cells. Four disease-causing genes have been identified: the ryanodine receptor 2 gene (RyR2) (60%), the cardiac calsequestrin 2 gene (CASQ2) (1-2%), the calmodulin gene (CALM1) (<1%) and the TRDM gene (<1%). Mutant RyR2 channels have a gain-of-function effect, resulting in excessive calcium release during sympathetic activation. Mutant CASQ2 causes loss of buffering capacity for calcium of the sarcoplasmatic reticulum. The mutations cause excessive calcium in the myocyte cytosol generating depolarizing membrane currents, which in turn lead to delayed afterdepolarizations and cardiac arrhythmias.
References
- Leenhardt A, Lucet V, Denjoy I, Grau F, Ngoc DD, and Coumel P. Catecholaminergic polymorphic ventricular tachycardia in children. A 7-year follow-up of 21 patients. Circulation. 1995 Mar 1;91(5):1512-9. DOI:10.1161/01.cir.91.5.1512 |
-
pmid-23022705
- van der Werf C, Kannankeril PJ, Sacher F, Krahn AD, Viskin S, Leenhardt A, Shimizu W, Sumitomo N, Fish FA, Bhuiyan ZA, Willems AR, van der Veen MJ, Watanabe H, Laborderie J, Haïssaguerre M, Knollmann BC, and Wilde AA. Flecainide therapy reduces exercise-induced ventricular arrhythmias in patients with catecholaminergic polymorphic ventricular tachycardia. J Am Coll Cardiol. 2011 May 31;57(22):2244-54. DOI:10.1016/j.jacc.2011.01.026 |
- Wilde AA, Bhuiyan ZA, Crotti L, Facchini M, De Ferrari GM, Paul T, Ferrandi C, Koolbergen DR, Odero A, and Schwartz PJ. Left cardiac sympathetic denervation for catecholaminergic polymorphic ventricular tachycardia. N Engl J Med. 2008 May 8;358(19):2024-9. DOI:10.1056/NEJMoa0708006 |
- van der Werf C and Wilde AA. Catecholaminergic polymorphic ventricular tachycardia: important messages from case reports. Europace. 2011 Jan;13(1):11-3. DOI:10.1093/europace/euq330 |
- Priori SG, Napolitano C, Memmi M, Colombi B, Drago F, Gasparini M, DeSimone L, Coltorti F, Bloise R, Keegan R, Cruz Filho FE, Vignati G, Benatar A, and DeLogu A. Clinical and molecular characterization of patients with catecholaminergic polymorphic ventricular tachycardia. Circulation. 2002 Jul 2;106(1):69-74. DOI:10.1161/01.cir.0000020013.73106.d8 |
- van der Werf C, Nederend I, Hofman N, van Geloven N, Ebink C, Frohn-Mulder IM, Alings AM, Bosker HA, Bracke FA, van den Heuvel F, Waalewijn RA, Bikker H, van Tintelen JP, Bhuiyan ZA, van den Berg MP, and Wilde AA. Familial evaluation in catecholaminergic polymorphic ventricular tachycardia: disease penetrance and expression in cardiac ryanodine receptor mutation-carrying relatives. Circ Arrhythm Electrophysiol. 2012 Aug 1;5(4):748-56. DOI:10.1161/CIRCEP.112.970517 |