Pulmonary Embolism: Difference between revisions
No edit summary |
No edit summary |
||
| (20 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
'' | ''James Heilman, MD, CCFP-EM. This text is currently a copy of the Pulmonary Embolism entry on Wikipedia'' | ||
'''Pulmonary embolism''' ('''PE''') is a blockage of the main artery of the lung or one of its branches by a substance that has travelled from elsewhere in the body through the bloodstream (embolism). Usually this is due to embolism of a thrombus (blood clot) from the |deep veins in the legs, a process termed venous thromboembolism. A small proportion is due to the embolization of air, fat, talc in drugs of intravenous drug abusers or amniotic fluid. The obstruction of the blood flow through the lungs and the resultant pressure on the right ventricle of the heart leads to the symptoms and signs of PE. The risk of PE is increased in various situations, such as cancer or prolonged bed rest.<cite>Goldhaber</cite> | |||
Diagnosis is based on these clinical findings in combination with laboratory tests (such as the | Symptoms of pulmonary embolism include difficulty breathing, chest pain on inspiration, and palpitations. Clinical signs include low blood oxygen saturation and cyanosis, rapid breathing, and a rapid heart rate. Severe cases of PE can lead to collapse, abnormally low blood pressure, and sudden death.<cite>Goldhaber</cite> | ||
Diagnosis is based on these clinical findings in combination with laboratory tests (such as the D-dimer test) and imaging studies, usually CT pulmonary angiography. Treatment is typically with anticoagulant medication, including heparin and warfarin. Severe cases may require thrombolysis with drugs such as tissue plasminogen activator (tPA) or may require surgical intervention via pulmonary thrombectomy.<cite>Goldhaber</cite> | |||
==Signs and symptoms== | ==Signs and symptoms== | ||
Symptoms of PE are sudden-onset | Symptoms of PE are sudden-onset dyspnea (shortness of breath), tachypnea (rapid breathing), chest pain of a "pleuritic" nature (worsened by breathing), cough and hemoptysis (coughing up blood). More severe cases can include signs such as cyanosis (blue discoloration, usually of the lips and fingers), collapse, and circulatory instability due to decreased blood flow through the lungs and into the left side of the heart. About 15% of all cases of sudden death are attributable to PE.<cite>Goldhaber</cite> | ||
On physical examination, the lungs are usually normal. Occasionally, a | On physical examination, the lungs are usually normal. Occasionally, a pleural friction rub may be audible over the affected area of the lung (mostly in PE with infarct) . A pleural effusion is sometimes present that is transudative, detectable by decreased percussion note, audible breath sounds and vocal resonance. Strain on the right ventricle may be detected as a left parasternal heave, a loud pulmonary component of the second heart sound, and raised jugular venous pressure.<cite>Goldhaber</cite> A low-grade fever may be present, particularly if there is associated pulmonary hemorrhage or infarction.<cite>Stein</cite> | ||
More rarely, inability of the right ventricle to remove fluid from the tissues leads to fluid accumulation in the legs (peripheral edema), congestion of the liver with mild | More rarely, inability of the right ventricle to remove fluid from the tissues leads to fluid accumulation in the legs (peripheral edema), congestion of the liver with mild jaundice and tenderness, and ascites (fluid in the abdominal cavity). | ||
==Risk factors== | ==Risk factors== | ||
The most common sources of embolism are | The most common sources of embolism are proximal leg deep venous thrombosis (DVTs) or pelvic vein thromboses. Any risk factor for DVT also increases the risk that the venous clot will dislodge and migrate to the lung circulation, which happens in up to 15% of all DVTs. The conditions are generally regarded as a continuum termed venous thromboembolism (VTE). | ||
The development of thrombosis is classically due to a group of causes named | The development of thrombosis is classically due to a group of causes named Virchow's triad (alterations in blood flow, factors in the vessel wall and factors affecting the properties of the blood). Often, more than one risk factor is present. | ||
* ''Alterations in blood flow'': immobilization (after surgery, | * ''Alterations in blood flow'': immobilization (after surgery, injury or long-distance air travel), pregnancy (also procoagulant), obesity (also procoagulant), cancer (also procoagulant) | ||
* ''Factors in the vessel wall'': of limited direct relevance in VTE | * ''Factors in the vessel wall'': of limited direct relevance in VTE | ||
* ''Factors affecting the properties of the blood'' (procoagulant state): | * ''Factors affecting the properties of the blood'' (procoagulant state): | ||
** | ** Estrogen-containing hormonal contraception | ||
** Genetic thrombophilia ( | ** Genetic thrombophilia (factor V Leiden, prothrombin mutation G20210A, protein C deficiency, protein S deficiency, antithrombin deficiency, hyperhomocysteinemia and plasminogen/fibrinolysis disorders) | ||
** Acquired thrombophilia ( | ** Acquired thrombophilia (antiphospholipid syndrome, nephrotic syndrome, paroxysmal nocturnal hemoglobinuria) | ||
** | ** Cancer]] (due to secretion of pro-coagulants) | ||
==Diagnosis== | ==Diagnosis== | ||
The diagnosis of PE is based primarily on validated clinical criteria combined with selective testing because the typical clinical presentation ( | The diagnosis of PE is based primarily on validated clinical criteria combined with selective testing because the typical clinical presentation (shortness of breath, chest pain) cannot be definitively differentiated from other causes of chest pain and shortness of breath. The decision to do medical imaging is usually based on clinical grounds, i.e. the medical history, symptoms and findings on physical examination, followed by an assessment of clinical probability.<cite>Goldhaber</cite> | ||
The most commonly used method to predict clinical probability, the Wells score, is a | The most commonly used method to predict clinical probability, the Wells score, is a clinical prediction rule, whose use is complicated by multiple versions being available. In 1995, Wells ''et al.'' initially developed a prediction rule (based on a literature search) to predict the likelihood of PE, based on clinical criteria.<cite>REFNAME1</cite> The prediction rule was revised in 1998 <cite>REFNAME2</cite> This prediction rule was further revised when simplified during a validation by Wells ''et al.'' in 2000. <cite>REFNAME3</cite> In the 2000 publication, Wells proposed two different scoring systems using cutoffs of 2 or 4 with the same prediction rule. <cite>REFNAME3</cite> In 2001, Wells published results using the more conservative cutoff of 2 to create three categories.<cite>REFNAME4</cite> An additional version, the "modified extended version", using the more recent cutoff of 2 but including findings from Wells's initial studies<cite>REFNAME5</cite> <cite>REFNAME6</cite> were proposed. <cite>REFNAME7</cite> Most recently, a further study reverted to Wells's earlier use of a cutoff of 4 points <cite>REFNAME3</cite> to create only two categories. <cite>REFNAME8</cite> | ||
There are additional prediction rules for PE, such as the | There are additional prediction rules for PE, such as the Geneva rule. More importantly, the use of ''any'' rule is associated with reduction in recurrent thromboembolism. <cite>REFNAME9</cite> | ||
''The Wells score'':< | ''The Wells score'': <cite>REFNAME10</cite> | ||
*clinically suspected | *clinically suspected DVT - 3.0 points | ||
*alternative diagnosis is less likely than PE - 3.0 points | *alternative diagnosis is less likely than PE - 3.0 points | ||
* | *tachycardia - 1.5 points | ||
*immobilization/surgery in previous four weeks - 1.5 points | *immobilization/surgery in previous four weeks - 1.5 points | ||
*history of | *history of DVT or PE - 1.5 points | ||
* | *hemoptysis - 1.0 points | ||
*malignancy (treatment for within 6 months, palliative) - 1.0 points | *malignancy (treatment for within 6 months, palliative) - 1.0 points | ||
Traditional interpretation< | Traditional interpretation <cite>REFNAME3</cite><cite>REFNAME4</cite> <cite>REFNAME11</cite> | ||
* Score >6.0 - High (probability 59% based on pooled data< | * Score >6.0 - High (probability 59% based on pooled data <cite>REFNAME12</cite>) | ||
* Score 2.0 to 6.0 - Moderate (probability 29% based on pooled data< | * Score 2.0 to 6.0 - Moderate (probability 29% based on pooled data <cite>REFNAME12</cite>) | ||
* Score <2.0 - Low (probability 15% based on pooled data< | * Score <2.0 - Low (probability 15% based on pooled data <cite>REFNAME12</cite>) | ||
Alternative interpretation< | Alternative interpretation <cite>REFNAME3</cite><cite>REFNAME8</cite> | ||
* Score > 4 - PE likely. Consider diagnostic imaging. | * Score > 4 - PE likely. Consider diagnostic imaging. | ||
* Score 4 or less - PE unlikely. Consider | * Score 4 or less - PE unlikely. Consider D-dimer to rule out PE. | ||
===Blood tests=== | ===Blood tests=== | ||
Early primary research has shown that in low/moderate suspicion of PE, a normal | Early primary research has shown that in low/moderate suspicion of PE, a normal D-dimer level (shown in a blood test) is enough to exclude the possibility of thrombotic PE. <cite>REFNAME13</cite> This has been corroborated by a recent systematic review of studies of patients with low pre-test probability (PTP) of PE and negative D-dimer results that found the three month risk of thromboembolic events in patients excluded in this manner was 0.14%, with 95% confidence intervals from 0.05 to 0.41%, though this review was limited by its use of only one randomized-controlled clinical trial, the remainder of studies being prospective cohorts. <cite>REFNAME14</cite> D-dimer is highly sensitive but not very specific (specificity around 50%). In other words, a positive D-dimer is not synonymous with PE, but a negative D-dimer is, with a good degree of certainty, an indication of absence of a PE. <cite>REFNAME15</cite> | ||
When a PE is being suspected, a number of | When a PE is being suspected, a number of blood tests are done, in order to exclude important secondary causes of PE. This includes a full blood count, clotting status (PT, aPTT, TT), and some screening tests (erythrocyte sedimentation rate, renal function, liver enzymes, electrolytes). If one of these is abnormal, further investigations might be warranted. | ||
===Imaging=== | ===Imaging=== | ||
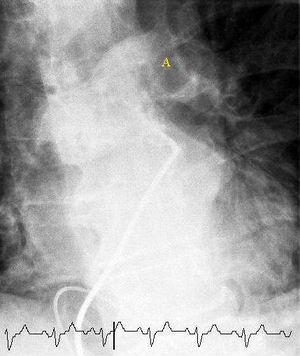
[[File:Pulmonary embolism selective angiogram.JPEG|thumb|Selective | [[File:Pulmonary embolism selective angiogram.JPEG|thumb|Selective pulmonary angiogram revealing significant thrombus (labelled A) causing a central obstruction in the left main pulmonary artery. ECG tracing shown at bottom.]] | ||
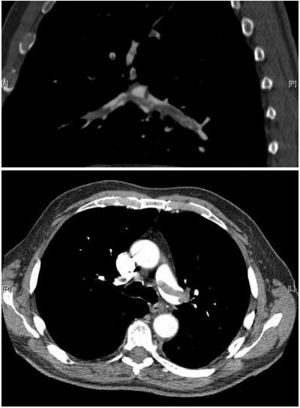
[[File:Pulmonary embolism CTPA.JPEG|thumb | [[File:Pulmonary embolism CTPA.JPEG|thumb|CT pulmonary angiography (CTPA) showing a saddle embolus and substantial thrombus burden in the lobar branches of both main pulmonary arteries.]] | ||
[[File:Pulmonary embolism scintigraphy PLoS.png|thumb| | [[File:Pulmonary embolism scintigraphy PLoS.png|thumb|Ventilation-perfusion scintigraphy in a woman taking hormonal contraceptives and valdecoxib.<br/>(A) After inhalation of 20.1 mCi of Xenon-133 gas, scintigraphic images were obtained in the posterior projection, showing uniform ventilation to lungs.<br/> | ||
(B) After intravenous injection of 4.1 mCi of | (B) After intravenous injection of 4.1 mCi of Technetium-99m-labeled macroaggregated albumin, scintigraphic images were obtained, shown here in the posterior projection. This and other views showed decreased activity in multiple regions.]] | ||
The | The gold standard for diagnosing pulmonary embolism (PE) is ''pulmonary angiography''. Pulmonary angiography is used less often due to wider acceptance of CT scans, which are non-invasive. CT pulmonary angiography is the recommended first line diagnostic imaging test in most people. | ||
;Non-invasive imaging | ;Non-invasive imaging | ||
CT pulmonary angiography (CTPA) is a pulmonary angiogram obtained using computed tomography (CT) with radiocontrast rather than right heart catheterization. Its advantages are clinical equivalence, its non-invasive nature, its greater availability to patients, and the possibility of identifying other lung disorders from the differential diagnosis in case there is no pulmonary embolism. Assessing the accuracy of CT pulmonary angiography is hindered by the rapid changes in the number of rows of detectors available in multidetector CT (MDCT) machines. <cite>REFNAME16</cite> According to a cohort study, single-slice spiral CT may help diagnose detection among patients with suspected pulmonary embolism. <cite>REFNAME17</cite> In this study, the sensitivity was 69% and specificity was 84%. In this study which had a prevalence of detection was 32%, the positive predictive value of 67.0% and negative predictive value of 85.2% ([http://medinformatics.uthscsa.edu/calculator/calc.shtml?calc_dx_SnSp.shtml?prevalence=32&sensitivity=69&specificity=84 click here] to adjust these results for patients at higher or lower risk of detection). However, this study's results may be biased due to possible incorporation bias, since the CT scan was the final diagnostic tool in patients with pulmonary embolism. The authors noted that a negative single slice CT scan is insufficient to rule out pulmonary embolism on its own. A separate study with a mixture of 4 slice and 16 slice scanners reported a sensitivity of 83% and a specificity of 96%. This study noted that additional testing is necessary when the clinical probability is inconsistent with the imaging results. <cite>REFNAME18</cite> CTPA is non-inferior to VQ scanning, and identifies more emboli (without necessarily improving the outcome) compared to VQ scanning. <cite>Anderson2007</cite> | |||
'' | ''Ventilation/perfusion scan'' (or ''V/Q scan'' or ''lung scintigraphy''), which shows that some areas of the lung are being ventilated but not perfused with blood (due to obstruction by a clot). This type of examination is used less often because of the more widespread availability of CT technology, however, it may be useful in patients who have an allergy to iodinated contrast or in pregnancy due to lower radiation exposure than CT. <cite>REFNAME19</cite> | ||
;Low probability diagnostic tests/non-diagnostic tests | ;Low probability diagnostic tests/non-diagnostic tests | ||
Tests that are frequently done that are not | Tests that are frequently done that are not sensitive for PE, but can be diagnostic. | ||
*'' | *''Chest X-rays'' are often done on patients with shortness of breath to help rule-out other causes, such as congestive heart failure and rib fracture. Chest X-rays in PE are rarely normal, <cite>REFNAME20</cite> but usually lack signs that suggest the diagnosis of PE (e.g. Westermark sign, Hampton's hump). | ||
*'' | *''Ultrasonography of the legs'', also known as ''leg doppler'', in search of deep venous thrombosis (DVT). The presence of DVT, as shown on ultrasonography of the legs, is in itself enough to warrant anticoagulation, without requiring the V/Q or spiral CT scans (because of the strong association between DVT and PE). This may be valid approach in pregnancy, in which the other modalities would increase the risk of birth defects in the unborn child. However, a negative scan does not rule out PE, and low-radiation dose scanning may be required if the mother is deemed at high risk of having pulmonary embolism. | ||
===Electrocardiogram=== | ===Electrocardiogram=== | ||
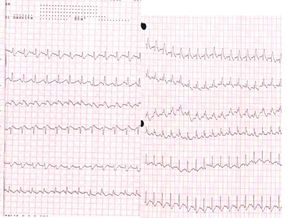
[[File:Pulmonary embolism ECG.jpg|thumb|Electrocardiogram of a patient with pulmonary embolism showing | [[File:Pulmonary embolism ECG.jpg|thumb|Electrocardiogram of a patient with pulmonary embolism showing sinus tachycardia of approximately 150 beats per minute and right bundle branch block.]] | ||
An | An electrocardiogram (ECG) is routinely done on patients with chest pain to quickly diagnose myocardial infarctions (heart attacks). An ECG may show signs of right heart strain or acute ''cor pulmonale'' in cases of large PEs - the classic signs are a large S wave in lead I, a large Q wave in lead III and an inverted T wave in lead III ("S1Q3T3"). <cite>McGinn</cite> This is occasionally (up to 20%) present, but may also occur in other acute lung conditions and has therefore limited diagnostic value. The most commonly seen signs in the ECG is sinus tachycardia, right axis deviation and right bundle branch block. <cite>REFNAME21</cite> Sinus tachycardia was however still only found in 8 - 69% of people with PE. <cite>REFNAME22</cite> | ||
===Echocardiography=== | ===Echocardiography=== | ||
In massive and submassive PE, dysfunction of the right side of the heart can be seen on | In massive and submassive PE, dysfunction of the right side of the heart can be seen on echocardiography, an indication that the pulmonary artery is severely obstructed and the heart is unable to match the pressure. Some studies (see below) suggest that this finding may be an indication for thrombolysis. Not every patient with a (suspected) pulmonary embolism requires an echocardiogram, but elevations in cardiac troponins or brain natriuretic peptide may indicate heart strain and warrant an echocardiogram. <cite>REFNAME23</cite> | ||
The specific appearance of the right ventricle on echocardiography is referred to as the ''McConnell's sign''. This is the finding of akinesia of the mid-free wall but normal motion of the apex. This phenomenon has a 77% sensitivity and a 94% specificity for the diagnosis of acute pulmonary embolism in the setting of right ventricular dysfunction.< | The specific appearance of the right ventricle on echocardiography is referred to as the ''McConnell's sign''. This is the finding of akinesia of the mid-free wall but normal motion of the apex. This phenomenon has a 77% sensitivity and a 94% specificity for the diagnosis of acute pulmonary embolism in the setting of right ventricular dysfunction. <cite>REFNAME24</cite> | ||
===Algorithms=== | ===Algorithms=== | ||
Recent recommendations for a diagnostic algorithm have been published by the PIOPED investigators; however, these recommendations do not reflect research using 64 slice MDCT.< | Recent recommendations for a diagnostic algorithm have been published by the PIOPED investigators; however, these recommendations do not reflect research using 64 slice MDCT. <cite>REFNAME25</cite> These investigators recommended: | ||
* Low clinical probability. If negative D-dimer, PE is excluded. If positive D-dimer, obtain MDCT and based treatment on results. | * Low clinical probability. If negative D-dimer, PE is excluded. If positive D-dimer, obtain MDCT and based treatment on results. | ||
* Moderate clinical probability. If negative D-dimer, PE is excluded. ''However'', the authors were not concerned that a negative MDCT with negative D-dimer in this setting has an 5% probability of being false. Presumably, the 5% error rate will fall as 64 slice MDCT is more commonly used. If positive D-dimer, obtain MDCT and based treatment on results. | * Moderate clinical probability. If negative D-dimer, PE is excluded. ''However'', the authors were not concerned that a negative MDCT with negative D-dimer in this setting has an 5% probability of being false. Presumably, the 5% error rate will fall as 64 slice MDCT is more commonly used. If positive D-dimer, obtain MDCT and based treatment on results. | ||
| Line 89: | Line 91: | ||
The Pulmonary Embolism Rule-out Criteria, or PERC rule, helps assess people in whom pulmonary embolism is suspected, but unlikely. Unlike the Wells Score and Geneva score, which are clinical prediction rules intended to risk stratify patients with suspected PE, the PERC rule is designed to rule out risk of PE in patients when the physician has already stratified them into a low-risk category. | The Pulmonary Embolism Rule-out Criteria, or PERC rule, helps assess people in whom pulmonary embolism is suspected, but unlikely. Unlike the Wells Score and Geneva score, which are clinical prediction rules intended to risk stratify patients with suspected PE, the PERC rule is designed to rule out risk of PE in patients when the physician has already stratified them into a low-risk category. | ||
Patients in this low risk category without any of these criteria may undergo no further diagnostic testing for PE: Hypoxia - Sa0<sub>2</sub> <95%, unilateral leg swelling, hemoptysis, prior DVT or PE, recent surgery or trauma, age >50, hormone use, tachycardia. The rationale behind this decision is that further testing (specifically CT angiogram of the chest) may cause more harm (from radiation exposure and contrast dye) than the risk of PE.< | Patients in this low risk category without any of these criteria may undergo no further diagnostic testing for PE: Hypoxia - Sa0<sub>2</sub> <95%, unilateral leg swelling, hemoptysis, prior DVT or PE, recent surgery or trauma, age >50, hormone use, tachycardia. The rationale behind this decision is that further testing (specifically CT angiogram of the chest) may cause more harm (from radiation exposure and contrast dye) than the risk of PE. <cite>REFNAME26</cite> The PERC rule has a sensitivity of 97.4% and specificity of 21.9% with a false negative rate of 1.0% (16/1666). <cite>REFNAME27</cite> | ||
==Treatment== | ==Treatment== | ||
In most cases, anticoagulant therapy is the mainstay of treatment. Acutely, supportive treatments, such as | In most cases, anticoagulant therapy is the mainstay of treatment. Acutely, supportive treatments, such as oxygen or analgesia, are often required. | ||
===Anticoagulation=== | ===Anticoagulation=== | ||
In most cases, anticoagulant therapy is the mainstay of treatment. Heparin, low molecular weight heparins (such as enoxaparin and dalteparin), or fondaparinux is administered initially, while warfarin, acenocoumarol, or phenprocoumon therapy is commenced (this may take several days, usually while the patient is in the hospital). Low molecular weight heparin may reduce bleeding among patients with pulmonary embolism as compared to heparin according to a systematic review of randomized controlled trials by the Cochrane Collaboration. <cite>REFNAME28</cite> The relative risk reduction was 40.0%. For patients at similar risk to those in this study (2.0% had bleeding when not treated with low molecular weight heparin), this leads to an absolute risk reduction of 0.8%. 125.0 patients must be treated for one to benefit. | |||
In most cases, | |||
It is possible to treat low risk patients (risk class I or class II) as | It is possible to treat low risk patients (risk class I or class II) as outpatients. <cite>Aujesky2011</cite> A randomised trial of 344 patients (171 outpatients and 168 inpatients) found that outcomes were equivalent whether patients were treated in hospital or at home (there was one death at 90 days in each group). <cite>Aujesky2011</cite> <cite>Aujesky2007</cite> This confirms the findings of an earlier systematic review of observational studies. <cite>REFNAME29</cite> | ||
Warfarin therapy often requires frequent dose adjustment and monitoring of the | Warfarin therapy often requires frequent dose adjustment and monitoring of the INR. In PE, INRs between 2.0 and 3.0 are generally considered ideal. If another episode of PE occurs under warfarin treatment, the INR window may be increased to e.g. 2.5-3.5 (unless there are contraindications) or anticoagulation may be changed to a different anticoagulant e.g. low molecular weight heparin. In patients with an underlying malignancy, therapy with a course of low molecular weight heparin may be favored over warfarin based on the results of the CLOT trial. <cite>REFNAME30</cite> | ||
Similarly, pregnant women are often maintained on low molecular weight heparin to avoid the known | Similarly, pregnant women are often maintained on low molecular weight heparin to avoid the known teratogenic effects of warfarin, especially in the early stages of pregnancy. | ||
People are usually admitted to hospital in the early stages of treatment, and tend to remain under inpatient care until INR has reached therapeutic levels. Increasingly, low-risk cases are managed on an outpatient basis in a fashion already common in the treatment of DVT.< | People are usually admitted to hospital in the early stages of treatment, and tend to remain under inpatient care until INR has reached therapeutic levels. Increasingly, low-risk cases are managed on an outpatient basis in a fashion already common in the treatment of DVT. <cite>REFNAME31</cite> | ||
Warfarin therapy is usually continued for 3–6 months, or "lifelong" if there have been previous DVTs or PEs, or none of the usual risk factors is present. An abnormal | Warfarin therapy is usually continued for 3–6 months, or "lifelong" if there have been previous DVTs or PEs, or none of the usual risk factors is present. An abnormal D-dimer level at the end of treatment might signal the need for continued treatment among patients with a first unprovoked pulmonary embolus. <cite>REFNAME32</cite> | ||
===Thrombolysis=== | ===Thrombolysis=== | ||
Massive PE causing hemodynamic instability (shock and/or hypotension, defined as a systolic blood pressure <90 mmHg or a pressure drop of 40 mmHg for>15 min if not caused by new-onset arrhythmia, hypovolemia or sepsis) is an indication for thrombolysis, the enzymatic destruction of the clot with medication. It is the best available medical treatment in this situation and is supported by clinical guidelines. <cite>REFNAME33</cite> <cite>ESC</cite> <cite>REFNAME34</cite> | |||
Massive PE causing hemodynamic instability (shock and/or hypotension, defined as a systolic blood pressure <90 mmHg or a pressure drop of 40 mmHg for>15 min if not caused by new-onset arrhythmia, hypovolemia or sepsis) is an indication for | |||
The use of thrombolysis in non-massive PEs is still debated. The aim of the therapy is to dissolve the clot, but there is an attendant risk of bleeding or | The use of thrombolysis in non-massive PEs is still debated. The aim of the therapy is to dissolve the clot, but there is an attendant risk of bleeding or stroke. <cite>REFNAME35</cite> The main indication for thrombolysis is in submassive PE where right ventricular dysfunction can be demonstrated on echocardiography, and the presence of visible thrombus in the atrium. <cite>REFNAME36</cite> | ||
===Surgery=== | ===Surgery=== | ||
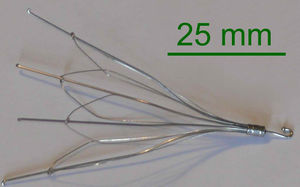
[[File:Inferior vena cava filter.jpg|thumb|right|Used inferior vena cava filter.]] | [[File:Inferior vena cava filter.jpg|thumb|right|Used inferior vena cava filter.]] | ||
Surgical management of acute pulmonary embolism ( | Surgical management of acute pulmonary embolism (pulmonary thrombectomy) is uncommon and has largely been abandoned because of poor long-term outcomes. However, recently, it has gone through a resurgence with the revision of the surgical technique and is thought to benefit selected patients. <cite>REFNAME37</cite> | ||
Chronic pulmonary embolism leading to | Chronic pulmonary embolism leading to pulmonary hypertension (known as ''chronic thromboembolic hypertension'') is treated with a surgical procedure known as a pulmonary thromboendarterectomy. | ||
===Inferior vena cava filter=== | ===Inferior vena cava filter=== | ||
If anticoagulant therapy is contraindicated and/or ineffective, or to prevent new emboli from entering the pulmonary artery and combining with an existing blockage, an inferior vena cava filter may be implanted. <cite>REFNAME38</cite> | |||
If anticoagulant therapy is | |||
==Prognosis== | ==Prognosis== | ||
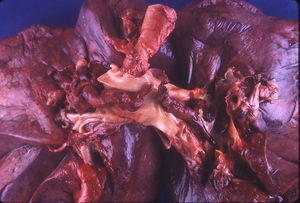
[[File:Saddle thromboembolus.jpg|thumb|Large saddle embolus seen at PA.]] | [[File:Saddle thromboembolus.jpg|thumb|Large saddle embolus seen at PA.]] | ||
Mortality from untreated PE is said to be 26%. This figure comes from a trial published in 1960 by Barrit and Jordan <cite>Barritt</cite>, which compared anticoagulation against placebo for the management of PE. Barritt and Jordan performed their study in the Bristol Royal Infirmary in 1957. This study is the only placebo controlled trial ever to examine the place of anticoagulants in the treatment of PE, the results of which were so convincing that the trial has never been repeated as to do so would be considered unethical. That said, the reported mortality rate of 26% in the placebo group is probably an overstatement, given that the technology of the day may have detected only severe PEs. | |||
Prognosis depends on the amount of lung that is affected and on the co-existence of other medical conditions; chronic embolisation to the lung can lead to | Prognosis depends on the amount of lung that is affected and on the co-existence of other medical conditions; chronic embolisation to the lung can lead to pulmonary hypertension. After a massive PE, the embolus must be resolved somehow if the patient is to survive. In thrombotic PE, the blood clot may be broken down by fibrinolysis, or it may be organized and recanalized so that a new channel forms through the clot. Blood flow is restored most rapidly in the first day or two after a PE. <cite>REFNAME39</cite> Improvement slows thereafter and some deficits may be permanent. There is controversy over whether or not small subsegmental PEs need to be treated at all <cite>REFNAME40</cite> and some evidence exists that patients with subsegmental PEs may do well without treatment. <cite>REFNAME41</cite> <cite>REFNAME42</cite> | ||
Once anticoagulation is stopped, the risk of a fatal pulmonary embolism is 0.5% per year.< | Once anticoagulation is stopped, the risk of a fatal pulmonary embolism is 0.5% per year. <cite>REFNAME43</cite> | ||
===Predicting mortality=== | ===Predicting mortality=== | ||
The PESI and Geneva prediction rules can estimate mortality and so may guide selection of patients who can be considered for outpatient therapy.< | The PESI and Geneva prediction rules can estimate mortality and so may guide selection of patients who can be considered for outpatient therapy. <cite>REFNAME44</cite> | ||
===Underlying causes=== | ===Underlying causes=== | ||
After a first PE, the search for secondary causes is usually brief. Only when a second PE occurs, and especially when this happens while still under | After a first PE, the search for secondary causes is usually brief. Only when a second PE occurs, and especially when this happens while still under anticoagulant therapy, a further search for underlying conditions is undertaken. This will include testing ("thrombophilia screen") for Factor V Leiden mutation, antiphospholipid antibodies, protein C and S and antithrombin levels, and later prothrombin mutation, MTHFR mutation, Factor VIII concentration and rarer inherited coagulation abnormalities. | ||
==References== | ==References== | ||
| Line 171: | Line 141: | ||
#Goldhaber isbn=0071391401 | #Goldhaber isbn=0071391401 | ||
#Stein pmid=19268750 | #Stein pmid=19268750 | ||
#REFNAME1 pmid=7752753 | |||
#REFNAME2 pmid=9867786 | |||
#REFNAME3 pmid=10744147 | |||
#REFNAME4 pmid=11453709 | |||
#REFNAME5 pmid=7752753 | |||
#REFNAME6 pmid=9867786 | |||
#REFNAME7 pmid=10739372 | |||
#REFNAME8 pmid=16403929 | |||
#REFNAME9 pmid=16461959 | |||
#REFNAME10 pmid=12952389 | |||
#REFNAME11 pmid=17874979 | |||
#REFNAME12 pmid=17185658 | |||
#REFNAME13 pmid=8165626 | |||
#REFNAME14 pmid=19404542 | |||
#REFNAME15 pmid=12928229 | |||
#REFNAME16 pmid=16479644 | |||
#REFNAME17 pmid=15634261 | |||
#REFNAME18 pmid=16738268 | |||
#Anderson2007 pmid=18165667 | |||
#REFNAME19 pmid=17322258 | |||
#REFNAME20 pmid=8372182 | |||
#McGinn McGinn S., White PD. Acute cor pulmonale resulting from pulmonary embolism. JAMA 1935:104:1473-80 | |||
#REFNAME21 pmid=11018210 | |||
#REFNAME22 isbn=1-4051-4166-2 | |||
#REFNAME23 pmid=14597581 | |||
#REFNAME24 pmid=8752195 | |||
#REFNAME25 pmid=17185658 | |||
#REFNAME26 pmid=15304025 | |||
#REFNAME27 pmid=18318689 | |||
#REFNAME28 pmid=15495007 | |||
#Aujesky2011 pmid=21703676 | |||
#Aujesky2007 Drahomir Aujesky, MD. Safety Study of Outpatient Treatment for Pulmonary Embolism (OTPE). NCT00425542 | |||
#REFNAME29 pmid=19407049 | |||
#REFNAME30 pmid=12853587 | |||
#REFNAME31 pmid=17567672 | |||
#REFNAME32 pmid=17065639 | |||
#REFNAME33 pmid=12775856 | |||
#ESC pmid=18757870 | |||
#REFNAME34 pmid=18574259 | |||
#REFNAME35 pmid=16625603 | |||
#REFNAME36 pmid=15094276 | |||
#REFNAME37 pmid=15339878 | |||
#REFNAME38 pmid=9459643 | |||
#Barritt pmid=13797091 | |||
#REFNAME39 pmid=5475816 | |||
#REFNAME40 pmid=16634736 | |||
#REFNAME41 pmid=16738268 | |||
#REFNAME42 pmid=16738276 | |||
#REFNAME43 pmid=18836122 | |||
#REFNAME44 pmid=17625081 | |||
</biblio> | </biblio> | ||
Latest revision as of 14:36, 5 December 2012
James Heilman, MD, CCFP-EM. This text is currently a copy of the Pulmonary Embolism entry on Wikipedia
Pulmonary embolism (PE) is a blockage of the main artery of the lung or one of its branches by a substance that has travelled from elsewhere in the body through the bloodstream (embolism). Usually this is due to embolism of a thrombus (blood clot) from the |deep veins in the legs, a process termed venous thromboembolism. A small proportion is due to the embolization of air, fat, talc in drugs of intravenous drug abusers or amniotic fluid. The obstruction of the blood flow through the lungs and the resultant pressure on the right ventricle of the heart leads to the symptoms and signs of PE. The risk of PE is increased in various situations, such as cancer or prolonged bed rest.[1]
Symptoms of pulmonary embolism include difficulty breathing, chest pain on inspiration, and palpitations. Clinical signs include low blood oxygen saturation and cyanosis, rapid breathing, and a rapid heart rate. Severe cases of PE can lead to collapse, abnormally low blood pressure, and sudden death.[1]
Diagnosis is based on these clinical findings in combination with laboratory tests (such as the D-dimer test) and imaging studies, usually CT pulmonary angiography. Treatment is typically with anticoagulant medication, including heparin and warfarin. Severe cases may require thrombolysis with drugs such as tissue plasminogen activator (tPA) or may require surgical intervention via pulmonary thrombectomy.[1]
Signs and symptoms
Symptoms of PE are sudden-onset dyspnea (shortness of breath), tachypnea (rapid breathing), chest pain of a "pleuritic" nature (worsened by breathing), cough and hemoptysis (coughing up blood). More severe cases can include signs such as cyanosis (blue discoloration, usually of the lips and fingers), collapse, and circulatory instability due to decreased blood flow through the lungs and into the left side of the heart. About 15% of all cases of sudden death are attributable to PE.[1]
On physical examination, the lungs are usually normal. Occasionally, a pleural friction rub may be audible over the affected area of the lung (mostly in PE with infarct) . A pleural effusion is sometimes present that is transudative, detectable by decreased percussion note, audible breath sounds and vocal resonance. Strain on the right ventricle may be detected as a left parasternal heave, a loud pulmonary component of the second heart sound, and raised jugular venous pressure.[1] A low-grade fever may be present, particularly if there is associated pulmonary hemorrhage or infarction.[2]
More rarely, inability of the right ventricle to remove fluid from the tissues leads to fluid accumulation in the legs (peripheral edema), congestion of the liver with mild jaundice and tenderness, and ascites (fluid in the abdominal cavity).
Risk factors
The most common sources of embolism are proximal leg deep venous thrombosis (DVTs) or pelvic vein thromboses. Any risk factor for DVT also increases the risk that the venous clot will dislodge and migrate to the lung circulation, which happens in up to 15% of all DVTs. The conditions are generally regarded as a continuum termed venous thromboembolism (VTE).
The development of thrombosis is classically due to a group of causes named Virchow's triad (alterations in blood flow, factors in the vessel wall and factors affecting the properties of the blood). Often, more than one risk factor is present.
- Alterations in blood flow: immobilization (after surgery, injury or long-distance air travel), pregnancy (also procoagulant), obesity (also procoagulant), cancer (also procoagulant)
- Factors in the vessel wall: of limited direct relevance in VTE
- Factors affecting the properties of the blood (procoagulant state):
- Estrogen-containing hormonal contraception
- Genetic thrombophilia (factor V Leiden, prothrombin mutation G20210A, protein C deficiency, protein S deficiency, antithrombin deficiency, hyperhomocysteinemia and plasminogen/fibrinolysis disorders)
- Acquired thrombophilia (antiphospholipid syndrome, nephrotic syndrome, paroxysmal nocturnal hemoglobinuria)
- Cancer]] (due to secretion of pro-coagulants)
Diagnosis
The diagnosis of PE is based primarily on validated clinical criteria combined with selective testing because the typical clinical presentation (shortness of breath, chest pain) cannot be definitively differentiated from other causes of chest pain and shortness of breath. The decision to do medical imaging is usually based on clinical grounds, i.e. the medical history, symptoms and findings on physical examination, followed by an assessment of clinical probability.[1]
The most commonly used method to predict clinical probability, the Wells score, is a clinical prediction rule, whose use is complicated by multiple versions being available. In 1995, Wells et al. initially developed a prediction rule (based on a literature search) to predict the likelihood of PE, based on clinical criteria.[3] The prediction rule was revised in 1998 [4] This prediction rule was further revised when simplified during a validation by Wells et al. in 2000. [5] In the 2000 publication, Wells proposed two different scoring systems using cutoffs of 2 or 4 with the same prediction rule. [5] In 2001, Wells published results using the more conservative cutoff of 2 to create three categories.[6] An additional version, the "modified extended version", using the more recent cutoff of 2 but including findings from Wells's initial studies[7] [8] were proposed. [9] Most recently, a further study reverted to Wells's earlier use of a cutoff of 4 points [5] to create only two categories. [10]
There are additional prediction rules for PE, such as the Geneva rule. More importantly, the use of any rule is associated with reduction in recurrent thromboembolism. [11]
The Wells score: [12]
- clinically suspected DVT - 3.0 points
- alternative diagnosis is less likely than PE - 3.0 points
- tachycardia - 1.5 points
- immobilization/surgery in previous four weeks - 1.5 points
- history of DVT or PE - 1.5 points
- hemoptysis - 1.0 points
- malignancy (treatment for within 6 months, palliative) - 1.0 points
Traditional interpretation [5][6] [13]
- Score >6.0 - High (probability 59% based on pooled data [14])
- Score 2.0 to 6.0 - Moderate (probability 29% based on pooled data [14])
- Score <2.0 - Low (probability 15% based on pooled data [14])
Alternative interpretation [5][10]
- Score > 4 - PE likely. Consider diagnostic imaging.
- Score 4 or less - PE unlikely. Consider D-dimer to rule out PE.
Blood tests
Early primary research has shown that in low/moderate suspicion of PE, a normal D-dimer level (shown in a blood test) is enough to exclude the possibility of thrombotic PE. [15] This has been corroborated by a recent systematic review of studies of patients with low pre-test probability (PTP) of PE and negative D-dimer results that found the three month risk of thromboembolic events in patients excluded in this manner was 0.14%, with 95% confidence intervals from 0.05 to 0.41%, though this review was limited by its use of only one randomized-controlled clinical trial, the remainder of studies being prospective cohorts. [16] D-dimer is highly sensitive but not very specific (specificity around 50%). In other words, a positive D-dimer is not synonymous with PE, but a negative D-dimer is, with a good degree of certainty, an indication of absence of a PE. [17]
When a PE is being suspected, a number of blood tests are done, in order to exclude important secondary causes of PE. This includes a full blood count, clotting status (PT, aPTT, TT), and some screening tests (erythrocyte sedimentation rate, renal function, liver enzymes, electrolytes). If one of these is abnormal, further investigations might be warranted.
Imaging
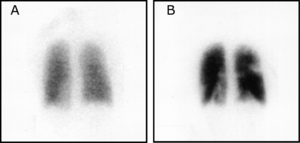
(A) After inhalation of 20.1 mCi of Xenon-133 gas, scintigraphic images were obtained in the posterior projection, showing uniform ventilation to lungs.
(B) After intravenous injection of 4.1 mCi of Technetium-99m-labeled macroaggregated albumin, scintigraphic images were obtained, shown here in the posterior projection. This and other views showed decreased activity in multiple regions.
The gold standard for diagnosing pulmonary embolism (PE) is pulmonary angiography. Pulmonary angiography is used less often due to wider acceptance of CT scans, which are non-invasive. CT pulmonary angiography is the recommended first line diagnostic imaging test in most people.
- Non-invasive imaging
CT pulmonary angiography (CTPA) is a pulmonary angiogram obtained using computed tomography (CT) with radiocontrast rather than right heart catheterization. Its advantages are clinical equivalence, its non-invasive nature, its greater availability to patients, and the possibility of identifying other lung disorders from the differential diagnosis in case there is no pulmonary embolism. Assessing the accuracy of CT pulmonary angiography is hindered by the rapid changes in the number of rows of detectors available in multidetector CT (MDCT) machines. [18] According to a cohort study, single-slice spiral CT may help diagnose detection among patients with suspected pulmonary embolism. [19] In this study, the sensitivity was 69% and specificity was 84%. In this study which had a prevalence of detection was 32%, the positive predictive value of 67.0% and negative predictive value of 85.2% (click here to adjust these results for patients at higher or lower risk of detection). However, this study's results may be biased due to possible incorporation bias, since the CT scan was the final diagnostic tool in patients with pulmonary embolism. The authors noted that a negative single slice CT scan is insufficient to rule out pulmonary embolism on its own. A separate study with a mixture of 4 slice and 16 slice scanners reported a sensitivity of 83% and a specificity of 96%. This study noted that additional testing is necessary when the clinical probability is inconsistent with the imaging results. [20] CTPA is non-inferior to VQ scanning, and identifies more emboli (without necessarily improving the outcome) compared to VQ scanning. [21]
Ventilation/perfusion scan (or V/Q scan or lung scintigraphy), which shows that some areas of the lung are being ventilated but not perfused with blood (due to obstruction by a clot). This type of examination is used less often because of the more widespread availability of CT technology, however, it may be useful in patients who have an allergy to iodinated contrast or in pregnancy due to lower radiation exposure than CT. [22]
- Low probability diagnostic tests/non-diagnostic tests
Tests that are frequently done that are not sensitive for PE, but can be diagnostic.
- Chest X-rays are often done on patients with shortness of breath to help rule-out other causes, such as congestive heart failure and rib fracture. Chest X-rays in PE are rarely normal, [23] but usually lack signs that suggest the diagnosis of PE (e.g. Westermark sign, Hampton's hump).
- Ultrasonography of the legs, also known as leg doppler, in search of deep venous thrombosis (DVT). The presence of DVT, as shown on ultrasonography of the legs, is in itself enough to warrant anticoagulation, without requiring the V/Q or spiral CT scans (because of the strong association between DVT and PE). This may be valid approach in pregnancy, in which the other modalities would increase the risk of birth defects in the unborn child. However, a negative scan does not rule out PE, and low-radiation dose scanning may be required if the mother is deemed at high risk of having pulmonary embolism.
Electrocardiogram
An electrocardiogram (ECG) is routinely done on patients with chest pain to quickly diagnose myocardial infarctions (heart attacks). An ECG may show signs of right heart strain or acute cor pulmonale in cases of large PEs - the classic signs are a large S wave in lead I, a large Q wave in lead III and an inverted T wave in lead III ("S1Q3T3"). [24] This is occasionally (up to 20%) present, but may also occur in other acute lung conditions and has therefore limited diagnostic value. The most commonly seen signs in the ECG is sinus tachycardia, right axis deviation and right bundle branch block. [25] Sinus tachycardia was however still only found in 8 - 69% of people with PE. [26]
Echocardiography
In massive and submassive PE, dysfunction of the right side of the heart can be seen on echocardiography, an indication that the pulmonary artery is severely obstructed and the heart is unable to match the pressure. Some studies (see below) suggest that this finding may be an indication for thrombolysis. Not every patient with a (suspected) pulmonary embolism requires an echocardiogram, but elevations in cardiac troponins or brain natriuretic peptide may indicate heart strain and warrant an echocardiogram. [27]
The specific appearance of the right ventricle on echocardiography is referred to as the McConnell's sign. This is the finding of akinesia of the mid-free wall but normal motion of the apex. This phenomenon has a 77% sensitivity and a 94% specificity for the diagnosis of acute pulmonary embolism in the setting of right ventricular dysfunction. [28]
Algorithms
Recent recommendations for a diagnostic algorithm have been published by the PIOPED investigators; however, these recommendations do not reflect research using 64 slice MDCT. [29] These investigators recommended:
- Low clinical probability. If negative D-dimer, PE is excluded. If positive D-dimer, obtain MDCT and based treatment on results.
- Moderate clinical probability. If negative D-dimer, PE is excluded. However, the authors were not concerned that a negative MDCT with negative D-dimer in this setting has an 5% probability of being false. Presumably, the 5% error rate will fall as 64 slice MDCT is more commonly used. If positive D-dimer, obtain MDCT and based treatment on results.
- High clinical probability. Proceed to MDCT. If positive, treat, if negative, additional tests are needed to exclude PE.
- Pulmonary Embolism Rule-out Criteria
The Pulmonary Embolism Rule-out Criteria, or PERC rule, helps assess people in whom pulmonary embolism is suspected, but unlikely. Unlike the Wells Score and Geneva score, which are clinical prediction rules intended to risk stratify patients with suspected PE, the PERC rule is designed to rule out risk of PE in patients when the physician has already stratified them into a low-risk category.
Patients in this low risk category without any of these criteria may undergo no further diagnostic testing for PE: Hypoxia - Sa02 <95%, unilateral leg swelling, hemoptysis, prior DVT or PE, recent surgery or trauma, age >50, hormone use, tachycardia. The rationale behind this decision is that further testing (specifically CT angiogram of the chest) may cause more harm (from radiation exposure and contrast dye) than the risk of PE. [30] The PERC rule has a sensitivity of 97.4% and specificity of 21.9% with a false negative rate of 1.0% (16/1666). [31]
Treatment
In most cases, anticoagulant therapy is the mainstay of treatment. Acutely, supportive treatments, such as oxygen or analgesia, are often required.
Anticoagulation
In most cases, anticoagulant therapy is the mainstay of treatment. Heparin, low molecular weight heparins (such as enoxaparin and dalteparin), or fondaparinux is administered initially, while warfarin, acenocoumarol, or phenprocoumon therapy is commenced (this may take several days, usually while the patient is in the hospital). Low molecular weight heparin may reduce bleeding among patients with pulmonary embolism as compared to heparin according to a systematic review of randomized controlled trials by the Cochrane Collaboration. [32] The relative risk reduction was 40.0%. For patients at similar risk to those in this study (2.0% had bleeding when not treated with low molecular weight heparin), this leads to an absolute risk reduction of 0.8%. 125.0 patients must be treated for one to benefit.
It is possible to treat low risk patients (risk class I or class II) as outpatients. [33] A randomised trial of 344 patients (171 outpatients and 168 inpatients) found that outcomes were equivalent whether patients were treated in hospital or at home (there was one death at 90 days in each group). [33] [34] This confirms the findings of an earlier systematic review of observational studies. [35]
Warfarin therapy often requires frequent dose adjustment and monitoring of the INR. In PE, INRs between 2.0 and 3.0 are generally considered ideal. If another episode of PE occurs under warfarin treatment, the INR window may be increased to e.g. 2.5-3.5 (unless there are contraindications) or anticoagulation may be changed to a different anticoagulant e.g. low molecular weight heparin. In patients with an underlying malignancy, therapy with a course of low molecular weight heparin may be favored over warfarin based on the results of the CLOT trial. [36]
Similarly, pregnant women are often maintained on low molecular weight heparin to avoid the known teratogenic effects of warfarin, especially in the early stages of pregnancy.
People are usually admitted to hospital in the early stages of treatment, and tend to remain under inpatient care until INR has reached therapeutic levels. Increasingly, low-risk cases are managed on an outpatient basis in a fashion already common in the treatment of DVT. [37]
Warfarin therapy is usually continued for 3–6 months, or "lifelong" if there have been previous DVTs or PEs, or none of the usual risk factors is present. An abnormal D-dimer level at the end of treatment might signal the need for continued treatment among patients with a first unprovoked pulmonary embolus. [38]
Thrombolysis
Massive PE causing hemodynamic instability (shock and/or hypotension, defined as a systolic blood pressure <90 mmHg or a pressure drop of 40 mmHg for>15 min if not caused by new-onset arrhythmia, hypovolemia or sepsis) is an indication for thrombolysis, the enzymatic destruction of the clot with medication. It is the best available medical treatment in this situation and is supported by clinical guidelines. [39] [40] [41]
The use of thrombolysis in non-massive PEs is still debated. The aim of the therapy is to dissolve the clot, but there is an attendant risk of bleeding or stroke. [42] The main indication for thrombolysis is in submassive PE where right ventricular dysfunction can be demonstrated on echocardiography, and the presence of visible thrombus in the atrium. [43]
Surgery
Surgical management of acute pulmonary embolism (pulmonary thrombectomy) is uncommon and has largely been abandoned because of poor long-term outcomes. However, recently, it has gone through a resurgence with the revision of the surgical technique and is thought to benefit selected patients. [44]
Chronic pulmonary embolism leading to pulmonary hypertension (known as chronic thromboembolic hypertension) is treated with a surgical procedure known as a pulmonary thromboendarterectomy.
Inferior vena cava filter
If anticoagulant therapy is contraindicated and/or ineffective, or to prevent new emboli from entering the pulmonary artery and combining with an existing blockage, an inferior vena cava filter may be implanted. [45]
Prognosis
Mortality from untreated PE is said to be 26%. This figure comes from a trial published in 1960 by Barrit and Jordan [46], which compared anticoagulation against placebo for the management of PE. Barritt and Jordan performed their study in the Bristol Royal Infirmary in 1957. This study is the only placebo controlled trial ever to examine the place of anticoagulants in the treatment of PE, the results of which were so convincing that the trial has never been repeated as to do so would be considered unethical. That said, the reported mortality rate of 26% in the placebo group is probably an overstatement, given that the technology of the day may have detected only severe PEs.
Prognosis depends on the amount of lung that is affected and on the co-existence of other medical conditions; chronic embolisation to the lung can lead to pulmonary hypertension. After a massive PE, the embolus must be resolved somehow if the patient is to survive. In thrombotic PE, the blood clot may be broken down by fibrinolysis, or it may be organized and recanalized so that a new channel forms through the clot. Blood flow is restored most rapidly in the first day or two after a PE. [47] Improvement slows thereafter and some deficits may be permanent. There is controversy over whether or not small subsegmental PEs need to be treated at all [48] and some evidence exists that patients with subsegmental PEs may do well without treatment. [49] [50]
Once anticoagulation is stopped, the risk of a fatal pulmonary embolism is 0.5% per year. [51]
Predicting mortality
The PESI and Geneva prediction rules can estimate mortality and so may guide selection of patients who can be considered for outpatient therapy. [52]
Underlying causes
After a first PE, the search for secondary causes is usually brief. Only when a second PE occurs, and especially when this happens while still under anticoagulant therapy, a further search for underlying conditions is undertaken. This will include testing ("thrombophilia screen") for Factor V Leiden mutation, antiphospholipid antibodies, protein C and S and antithrombin levels, and later prothrombin mutation, MTHFR mutation, Factor VIII concentration and rarer inherited coagulation abnormalities.
References
- ISBN:0071391401
- Stein PD, Sostman HD, Hull RD, Goodman LR, Leeper KV Jr, Gottschalk A, Tapson VF, and Woodard PK. Diagnosis of pulmonary embolism in the coronary care unit. Am J Cardiol. 2009 Mar 15;103(6):881-6. DOI:10.1016/j.amjcard.2008.11.040 |
- Wells PS, Hirsh J, Anderson DR, Lensing AW, Foster G, Kearon C, Weitz J, D'Ovidio R, Cogo A, and Prandoni P. Accuracy of clinical assessment of deep-vein thrombosis. Lancet. 1995 May 27;345(8961):1326-30. DOI:10.1016/s0140-6736(95)92535-x |
- Wells PS, Ginsberg JS, Anderson DR, Kearon C, Gent M, Turpie AG, Bormanis J, Weitz J, Chamberlain M, Bowie D, Barnes D, and Hirsh J. Use of a clinical model for safe management of patients with suspected pulmonary embolism. Ann Intern Med. 1998 Dec 15;129(12):997-1005. DOI:10.7326/0003-4819-129-12-199812150-00002 |
- Wells PS, Anderson DR, Rodger M, Ginsberg JS, Kearon C, Gent M, Turpie AG, Bormanis J, Weitz J, Chamberlain M, Bowie D, Barnes D, and Hirsh J. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000 Mar;83(3):416-20.
- Wells PS, Anderson DR, Rodger M, Stiell I, Dreyer JF, Barnes D, Forgie M, Kovacs G, Ward J, and Kovacs MJ. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer. Ann Intern Med. 2001 Jul 17;135(2):98-107. DOI:10.7326/0003-4819-135-2-200107170-00010 |
- Wells PS, Hirsh J, Anderson DR, Lensing AW, Foster G, Kearon C, Weitz J, D'Ovidio R, Cogo A, and Prandoni P. Accuracy of clinical assessment of deep-vein thrombosis. Lancet. 1995 May 27;345(8961):1326-30. DOI:10.1016/s0140-6736(95)92535-x |
- Wells PS, Ginsberg JS, Anderson DR, Kearon C, Gent M, Turpie AG, Bormanis J, Weitz J, Chamberlain M, Bowie D, Barnes D, and Hirsh J. Use of a clinical model for safe management of patients with suspected pulmonary embolism. Ann Intern Med. 1998 Dec 15;129(12):997-1005. DOI:10.7326/0003-4819-129-12-199812150-00002 |
- Sanson BJ, Lijmer JG, Mac Gillavry MR, Turkstra F, Prins MH, and Büller HR. Comparison of a clinical probability estimate and two clinical models in patients with suspected pulmonary embolism. ANTELOPE-Study Group. Thromb Haemost. 2000 Feb;83(2):199-203.
- van Belle A, Büller HR, Huisman MV, Huisman PM, Kaasjager K, Kamphuisen PW, Kramer MH, Kruip MJ, Kwakkel-van Erp JM, Leebeek FW, Nijkeuter M, Prins MH, Sohne M, Tick LW, and Christopher Study Investigators. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computed tomography. JAMA. 2006 Jan 11;295(2):172-9. DOI:10.1001/jama.295.2.172 |
- Roy PM, Meyer G, Vielle B, Le Gall C, Verschuren F, Carpentier F, Leveau P, Furber A, and EMDEPU Study Group. Appropriateness of diagnostic management and outcomes of suspected pulmonary embolism. Ann Intern Med. 2006 Feb 7;144(3):157-64. DOI:10.7326/0003-4819-144-3-200602070-00003 |
- Neff MJ and ACEP. ACEP releases clinical policy on evaluation and management of pulmonary embolism. Am Fam Physician. 2003 Aug 15;68(4):759-60.
- Yap KS, Kalff V, Turlakow A, and Kelly MJ. A prospective reassessment of the utility of the Wells score in identifying pulmonary embolism. Med J Aust. 2007 Sep 17;187(6):333-6. DOI:10.5694/j.1326-5377.2007.tb01274.x |
- Stein PD, Woodard PK, Weg JG, Wakefield TW, Tapson VF, Sostman HD, Sos TA, Quinn DA, Leeper KV Jr, Hull RD, Hales CA, Gottschalk A, Goodman LR, Fowler SE, Buckley JD, and PIOPED II Investigators. Diagnostic pathways in acute pulmonary embolism: recommendations of the PIOPED II Investigators. Radiology. 2007 Jan;242(1):15-21. DOI:10.1148/radiol.2421060971 |
- Bounameaux H, de Moerloose P, Perrier A, and Reber G. Plasma measurement of D-dimer as diagnostic aid in suspected venous thromboembolism: an overview. Thromb Haemost. 1994 Jan;71(1):1-6.
- Carrier M, Righini M, Djurabi RK, Huisman MV, Perrier A, Wells PS, Rodger M, Wuillemin WA, and Le Gal G. VIDAS D-dimer in combination with clinical pre-test probability to rule out pulmonary embolism. A systematic review of management outcome studies. Thromb Haemost. 2009 May;101(5):886-92.
- Schrecengost JE, LeGallo RD, Boyd JC, Moons KG, Gonias SL, Rose CE Jr, and Bruns DE. Comparison of diagnostic accuracies in outpatients and hospitalized patients of D-dimer testing for the evaluation of suspected pulmonary embolism. Clin Chem. 2003 Sep;49(9):1483-90. DOI:10.1373/49.9.1483 |
- Schaefer-Prokop C and Prokop M. MDCT for the diagnosis of acute pulmonary embolism. Eur Radiol. 2005 Nov;15 Suppl 4:D37-41. DOI:10.1007/s10406-005-0144-3 |
- Van Strijen MJ, De Monye W, Kieft GJ, Pattynama PM, Prins MH, and Huisman MV. Accuracy of single-detector spiral CT in the diagnosis of pulmonary embolism: a prospective multicenter cohort study of consecutive patients with abnormal perfusion scintigraphy. J Thromb Haemost. 2005 Jan;3(1):17-25. DOI:10.1111/j.1538-7836.2004.01064.x |
- Stein PD, Fowler SE, Goodman LR, Gottschalk A, Hales CA, Hull RD, Leeper KV Jr, Popovich J Jr, Quinn DA, Sos TA, Sostman HD, Tapson VF, Wakefield TW, Weg JG, Woodard PK, and PIOPED II Investigators. Multidetector computed tomography for acute pulmonary embolism. N Engl J Med. 2006 Jun 1;354(22):2317-27. DOI:10.1056/NEJMoa052367 |
- Anderson DR, Kahn SR, Rodger MA, Kovacs MJ, Morris T, Hirsch A, Lang E, Stiell I, Kovacs G, Dreyer J, Dennie C, Cartier Y, Barnes D, Burton E, Pleasance S, Skedgel C, O'Rouke K, and Wells PS. Computed tomographic pulmonary angiography vs ventilation-perfusion lung scanning in patients with suspected pulmonary embolism: a randomized controlled trial. JAMA. 2007 Dec 19;298(23):2743-53. DOI:10.1001/jama.298.23.2743 |
- Scarsbrook AF and Gleeson FV. Investigating suspected pulmonary embolism in pregnancy. BMJ. 2007 Feb 24;334(7590):418-9. DOI:10.1136/bmj.39071.617257.80 |
- Worsley DF, Alavi A, Aronchick JM, Chen JT, Greenspan RH, and Ravin CE. Chest radiographic findings in patients with acute pulmonary embolism: observations from the PIOPED Study. Radiology. 1993 Oct;189(1):133-6. DOI:10.1148/radiology.189.1.8372182 |
-
McGinn S., White PD. Acute cor pulmonale resulting from pulmonary embolism. JAMA 1935:104:1473-80
- Rodger M, Makropoulos D, Turek M, Quevillon J, Raymond F, Rasuli P, and Wells PS. Diagnostic value of the electrocardiogram in suspected pulmonary embolism. Am J Cardiol. 2000 Oct 1;86(7):807-9, A10. DOI:10.1016/s0002-9149(00)01090-0 |
- ISBN:1-4051-4166-2
- Kucher N and Goldhaber SZ. Cardiac biomarkers for risk stratification of patients with acute pulmonary embolism. Circulation. 2003 Nov 4;108(18):2191-4. DOI:10.1161/01.CIR.0000100687.99687.CE |
- McConnell MV, Solomon SD, Rayan ME, Come PC, Goldhaber SZ, and Lee RT. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol. 1996 Aug 15;78(4):469-73. DOI:10.1016/s0002-9149(96)00339-6 |
- Stein PD, Woodard PK, Weg JG, Wakefield TW, Tapson VF, Sostman HD, Sos TA, Quinn DA, Leeper KV Jr, Hull RD, Hales CA, Gottschalk A, Goodman LR, Fowler SE, Buckley JD, and PIOPED II Investigators. Diagnostic pathways in acute pulmonary embolism: recommendations of the PIOPED II Investigators. Radiology. 2007 Jan;242(1):15-21. DOI:10.1148/radiol.2421060971 |
- Kline JA, Mitchell AM, Kabrhel C, Richman PB, and Courtney DM. Clinical criteria to prevent unnecessary diagnostic testing in emergency department patients with suspected pulmonary embolism. J Thromb Haemost. 2004 Aug;2(8):1247-55. DOI:10.1111/j.1538-7836.2004.00790.x |
- Kline JA, Courtney DM, Kabrhel C, Moore CL, Smithline HA, Plewa MC, Richman PB, O'Neil BJ, and Nordenholz K. Prospective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008 May;6(5):772-80. DOI:10.1111/j.1538-7836.2008.02944.x |
- van Dongen CJ, van den Belt AG, Prins MH, and Lensing AW. Fixed dose subcutaneous low molecular weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism. Cochrane Database Syst Rev. 2004 Oct 18(4):CD001100. DOI:10.1002/14651858.CD001100.pub2 |
- Aujesky D, Roy PM, Verschuren F, Righini M, Osterwalder J, Egloff M, Renaud B, Verhamme P, Stone RA, Legall C, Sanchez O, Pugh NA, N'gako A, Cornuz J, Hugli O, Beer HJ, Perrier A, Fine MJ, and Yealy DM. Outpatient versus inpatient treatment for patients with acute pulmonary embolism: an international, open-label, randomised, non-inferiority trial. Lancet. 2011 Jul 2;378(9785):41-8. DOI:10.1016/S0140-6736(11)60824-6 |
-
Drahomir Aujesky, MD. Safety Study of Outpatient Treatment for Pulmonary Embolism (OTPE). NCT00425542
- Squizzato A, Galli M, Dentali F, and Ageno W. Outpatient treatment and early discharge of symptomatic pulmonary embolism: a systematic review. Eur Respir J. 2009 May;33(5):1148-55. DOI:10.1183/09031936.00133608 |
- Lee AY, Levine MN, Baker RI, Bowden C, Kakkar AK, Prins M, Rickles FR, Julian JA, Haley S, Kovacs MJ, Gent M, and Randomized Comparison of Low-Molecular-Weight Heparin versus Oral Anticoagulant Therapy for the Prevention of Recurrent Venous Thromboembolism in Patients with Cancer (CLOT) Investigators. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003 Jul 10;349(2):146-53. DOI:10.1056/NEJMoa025313 |
- Davies CW, Wimperis J, Green ES, Pendry K, Killen J, Mehdi I, Tiplady C, Kesteven P, Rose P, and Oldfield W. Early discharge of patients with pulmonary embolism: a two-phase observational study. Eur Respir J. 2007 Oct;30(4):708-14. DOI:10.1183/09031936.00140506 |
- Palareti G, Cosmi B, Legnani C, Tosetto A, Brusi C, Iorio A, Pengo V, Ghirarduzzi A, Pattacini C, Testa S, Lensing AW, Tripodi A, and PROLONG Investigators. D-dimer testing to determine the duration of anticoagulation therapy. N Engl J Med. 2006 Oct 26;355(17):1780-9. DOI:10.1056/NEJMoa054444 |
- British Thoracic Society Standards of Care Committee Pulmonary Embolism Guideline Development Group. British Thoracic Society guidelines for the management of suspected acute pulmonary embolism. Thorax. 2003 Jun;58(6):470-83. DOI:10.1136/thorax.58.6.470 |
- Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P, Bengel F, Brady AJ, Ferreira D, Janssens U, Klepetko W, Mayer E, Remy-Jardin M, Bassand JP, and ESC Committee for Practice Guidelines (CPG). Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Eur Heart J. 2008 Sep;29(18):2276-315. DOI:10.1093/eurheartj/ehn310 |
- Hirsh J, Guyatt G, Albers GW, Harrington R, and Schünemann HJ. Executive summary: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008 Jun;133(6 Suppl):71S-109S. DOI:10.1378/chest.08-0693 |
- Dong B, Jirong Y, Liu G, Wang Q, and Wu T. Thrombolytic therapy for pulmonary embolism. Cochrane Database Syst Rev. 2006 Apr 19(2):CD004437. DOI:10.1002/14651858.CD004437.pub2 |
- Goldhaber SZ. Pulmonary embolism. Lancet. 2004 Apr 17;363(9417):1295-305. DOI:10.1016/S0140-6736(04)16004-2 |
- Augustinos P and Ouriel K. Invasive approaches to treatment of venous thromboembolism. Circulation. 2004 Aug 31;110(9 Suppl 1):I27-34. DOI:10.1161/01.CIR.0000140900.64198.f4 |
- Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, Laporte S, Faivre R, Charbonnier B, Barral FG, Huet Y, and Simonneau G. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med. 1998 Feb 12;338(7):409-15. DOI:10.1056/NEJM199802123380701 |
- BARRITT DW and JORDAN SC. Anticoagulant drugs in the treatment of pulmonary embolism. A controlled trial. Lancet. 1960 Jun 18;1(7138):1309-12. DOI:10.1016/s0140-6736(60)92299-6 |
- Walker RH, Goodwin J, and Jackson JA. Resolution of pulmonary embolism. Br Med J. 1970 Oct 17;4(5728):135-9. DOI:10.1136/bmj.4.5728.135 |
- Le Gal G, Righini M, Parent F, van Strijen M, and Couturaud F. Diagnosis and management of subsegmental pulmonary embolism. J Thromb Haemost. 2006 Apr;4(4):724-31. DOI:10.1111/j.1538-7836.2006.01819.x |
- Stein PD, Fowler SE, Goodman LR, Gottschalk A, Hales CA, Hull RD, Leeper KV Jr, Popovich J Jr, Quinn DA, Sos TA, Sostman HD, Tapson VF, Wakefield TW, Weg JG, Woodard PK, and PIOPED II Investigators. Multidetector computed tomography for acute pulmonary embolism. N Engl J Med. 2006 Jun 1;354(22):2317-27. DOI:10.1056/NEJMoa052367 |
- Perrier A and Bounameaux H. Accuracy or outcome in suspected pulmonary embolism. N Engl J Med. 2006 Jun 1;354(22):2383-5. DOI:10.1056/NEJMe068076 |
- White RH. Risk of fatal pulmonary embolism was 0.49 per 100 person-years after discontinuing anticoagulant therapy for venous thromboembolism. Evid Based Med. 2008 Oct;13(5):154. DOI:10.1136/ebm.13.5.154 |
- Jiménez D, Yusen RD, Otero R, Uresandi F, Nauffal D, Laserna E, Conget F, Oribe M, Cabezudo MA, and Díaz G. Prognostic models for selecting patients with acute pulmonary embolism for initial outpatient therapy. Chest. 2007 Jul;132(1):24-30. DOI:10.1378/chest.06-2921 |