Chest Pain / Angina Pectoris: Difference between revisions
Secretariat (talk | contribs) |
Secretariat (talk | contribs) No edit summary |
||
| Line 6: | Line 6: | ||
===History=== | ===History=== | ||
Patients often experience angina pectoris as if a elephant stands on their chest. Because the heart itself has very few nerves the pain can be sensible elsewhere in the upper body, mainly arms, jaw and/or back.<cite>Foreman</cite> Some patients only complain about stomach ache so the presentation can be very a specific.<cite>Canto</cite> <cite>Pope</cite> | Patients often experience angina pectoris as if a elephant stands on their chest. Because the heart itself has very few nerves the pain can be sensible elsewhere in the upper body, mainly arms, jaw and/or back.<cite>Foreman</cite> Some patients only complain about stomach ache so the presentation can be very a specific.<cite>Canto</cite>,<cite>Pope</cite> | ||
Angina pectoris however has some characteristics that can help to differentiate between other causes of (chest) pain. Angina pectoris is gradual in onset and offset, with the intensity increasing and decreasing over several minutes. The pain is constant and does not change with respiration or position. If patients had angina pectoris before they will recognize the pain immediately.<cite>Constant</cite> | Angina pectoris however has some characteristics that can help to differentiate between other causes of (chest) pain. Angina pectoris is gradual in onset and offset, with the intensity increasing and decreasing over several minutes. The pain is constant and does not change with respiration or position. If patients had angina pectoris before they will recognize the pain immediately.<cite>Constant</cite> | ||
| Line 27: | Line 27: | ||
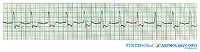
===ECG=== | ===ECG=== | ||
[[File:TBC00003.jpg|200px|thumb|right|]] | [[File:TBC00003.jpg|200px|thumb|right|]] | ||
The electrocardiogram (ECG) is an easy and important tool to differentiate between myocardial ischemia and infarction. Patients with unstable angina pectoris will show abnormalities on the ECG at rest, in particular ST depression. | The electrocardiogram (ECG) is an easy and important tool to differentiate between myocardial ischemia and infarction. Patients with unstable angina pectoris will show abnormalities on the ECG at rest, in particular ST depression. | ||
Patients with stable angina pectoris are likely to have a completely normal ECG at rest, exercise ECG testing will be necessary to show any abnormalities. During exercise ECG testing an ECG is made during cycling on a home trainer or walking on a treadmill. While exercising the oxygen demand of the heart increases, if the narrowed coronary arteries are unable to supply enough oxygenated blood, the patient develops pain on the chest and the ECG will show abnormalities.<cite>Fox</cite> | Patients with stable angina pectoris are likely to have a completely normal ECG at rest, exercise ECG testing will be necessary to show any abnormalities.<cite>Ref1</cite> During exercise ECG testing an ECG is made during cycling on a home trainer or walking on a treadmill. While exercising the oxygen demand of the heart increases, if the narrowed coronary arteries are unable to supply enough oxygenated blood, the patient develops pain on the chest and the ECG will show abnormalities.<cite>Fox</cite> | ||
===Additional Research=== | ===Additional Research=== | ||
| Line 39: | Line 38: | ||
The findings on stress testing can be used to determine the choice between medical therapy and revascularization in patients with stable angina. Coronary angiography is recommended based upon symptoms, left ventricular function, and estimated risk by stress testing.<cite>Fraker</cite> | The findings on stress testing can be used to determine the choice between medical therapy and revascularization in patients with stable angina. Coronary angiography is recommended based upon symptoms, left ventricular function, and estimated risk by stress testing.<cite>Fraker</cite> | ||
== | '''Table 1''' | ||
In | |||
==Coronary Angiography== | |||
In patients with unstable angina pectoris early coronary angiography possibly followed by revascularization is usually performed within 4 to 24 hours of admission in the hospital. In most clinical trials this strategy has shown a reduction in the incidence of death or nonfatal myocardial infraction.<cite>Anderson2</cite> | |||
A CAG is an X ray examination of the coronary arteries, a catheter is inserted into the femoral artery or into the radial artery. The tip of the catheter is positioned at the beginning of the coronary arteries and contrast fluid is injected. Contrast is visible by X ray and the images that are obtained are called angiograms. | |||
On an angiogram stenoses will be visible, if the stenosis is significant coronary intervention will take place. Ideally this happens immediately following the CAG but not all hospitals that are entitled to carry out CAG are qualified to perform percutaneous coronary intervention (PCI). | |||
==Treatment== | ==Treatment== | ||
===Medication=== | ===Medication=== | ||
In patients with stable angina pectoris | In patients with stable angina pectoris percutaneous coronary intervention does not offer any benefit in terms of death, myocardial infarction, or the need for subsequent revascularization compared with conservative medical treatment.<cite>Katritsis</cite> | ||
Initial treatment of stable angina pectoris therefore focuses on medication to keep the workload of the heart as low as possible. β blockers lower heart rate and blood pressure, this decreases the oxygen demand of the heart.<cite>Garcia</cite> Nitrates dilatate the coronary arteries so the heart receives more oxygenated blood.<cite>Abrams2</cite> Anticoagulants (aspirin) to reduce the risk of development of a thrombus in the coronary arteries.<cite>Hennekens</cite> | |||
Apart from starting medication the patient needs to minimize any present risk factors like smoking, overweight and drinking alcohol. ''See chronic coronary diseases''. | |||
==Percutaneous Coronary Intervention== | |||
The procedure of PCI is similar to a CAG, except this time a catheter with an inflatable balloon will be brought at the site of the stenosis. Inflation of the balloon within the coronary artery will crush the atherosclerosis and eliminate the stenosis. To prevent that the effect of the balloon is only temporarily a stent is often positioned at the site of the stenosis. | The procedure of PCI is similar to a CAG, except this time a catheter with an inflatable balloon will be brought at the site of the stenosis. Inflation of the balloon within the coronary artery will crush the atherosclerosis and eliminate the stenosis. To prevent that the effect of the balloon is only temporarily a stent is often positioned at the site of the stenosis. | ||
==Coronary Artery Bypass Graft== | |||
There are circumstances in which CABG should be performed. | |||
CABG | |||
{| class="wikitable" border="1" style="width: 700px" | {| class="wikitable" border="1" style="width: 700px" | ||
| Line 84: | Line 78: | ||
|- | |- | ||
| colspan="2" | Class I - There is evidence and/or general agreement that CABG should be performed in patients with STEMI in the following settings. | | colspan="2" | Class I - There is evidence and/or general agreement that CABG should be performed in patients with STEMI in the following settings. | ||
|} | |||
CABG does not eliminate the stenosis like PCI does. Using the internal thoracic arteries or the saphenous veins from the legs a bypass is made around the stenosis. The bypass originates from the aorta and terminates directly after the stenosis. Thereby restoring the blood supply to the ramifications. | |||
=Myocardial Infarction= | |||
In 2006 425.425 people died from a heart attack, 1.255.000 new and recurrent coronary attacks took place, about 34% died, 17.600.000 victims of angina, heart attack and other forms of coronary heart disease are still living. | |||
These numbers only account for the United States. | |||
==Pathofysiology== | |||
A heart attack or myocardial infarction (MI) is an acute presentation of a process that has been going on much longer. The process responsible is atherosclerosis. Atherosclerosis is a chronic disease of the arteries in which artery walls thicken by deposition of fatty materials such as cholesterol. The result over decades are plaques, which can narrow the lumen of the arteries significantly and progressively causing symptoms as angina pectoris. Plaques can also suddenly rupture, trigger a cascade which results in a thrombus and thereby cause myocardial infarction.<cite>Davies3</cite> | |||
==History== | |||
Classic presentation of a myocardial infarction is acute chest pain which lasts longer than a few minutes. PMID 16304077 The pain does not decrease at rest and is only temporarily relieved with nitroglycerin. Common accompanying symptoms are radiating pain to shoulder, arm, back and/or jaw. PMID 10099685 Shortness of breath can occur, as well as sweating, fainting, nausea and vomiting, so called vegetative symptoms. Some patients not really complain about chest pain but more about abdominal pain so as with angina pectoris the presentation can be very a specific. PMID 10866870, PMID 10751787 | |||
It is important to complete the history with information about past history (prior history of ischemic events or vascular disease), risk factors for cardiovascular disease (o.a. smoking, hypertension, hyperlipidemia, obesity) and family history (direct family with myocardial infarction and/or sudden cardiac death). | |||
Signs of heart failure such as orthopnea (not able to sleep without a pillow), progressive dyspnoea and oedematous ankles are indicative for the extent of the problem. PMID 15289388 | |||
A suspected myocardial infarction should be rapidly evaluated to initiate appropriate therapy. | |||
==Physical Examination== | |||
On physical examination evidence of systemic hypoperfusion can be found such as hypotension, tachycardia, impaired cognition, pale and ashen skin. PMID 15289388 | |||
If during auscultation pulmonary crackles are heard and pitting oedema of the ankles is seen heart failure is complicating the myocardial infarction. | |||
History and physical examination are helpful to determine myocardial infarction as diagnosis and to exclude other causes of chest pain, such as angina pectoris, aorta dissection, arrhythmias, pulmonary embolism, pneumonia, heartburn, hyperventilation or musculoskeletal problems. PMID 15289388 | |||
==References== | ==References== | ||
| Line 96: | Line 117: | ||
#Constant pmid=6831781 | #Constant pmid=6831781 | ||
#Anderson pmid=17692738 | #Anderson pmid=17692738 | ||
#Anderson2 pmid=17692738 | |||
#Abrams pmid=3925741 | #Abrams pmid=3925741 | ||
#Abrams2 pmid=3925741 | |||
#Henrikson pmid=14678917 | #Henrikson pmid=14678917 | ||
#Antman pmid=15289388 | #Antman pmid=15289388 | ||
| Line 105: | Line 128: | ||
#Kwong pmid=12566362 | #Kwong pmid=12566362 | ||
#Fraker pmid=18061078 | #Fraker pmid=18061078 | ||
#Katritsis pmid=15927966 | |||
#Garcia pmid=16735367 | |||
#Hennekens pmid=9355934 | |||
#Davies3 pmid=11084798 | |||
#Ref1 pmid=8375424 | |||
</biblio> | </biblio> | ||
Revision as of 10:11, 10 August 2011
In 1772 doctor William Heberden first described angina pectoris, he wrote: “They who are afflicted with it are seized, while they are walking (more especially if it be up hill), with a painful and most disagreeable sensation in the breast, which seems as if it would extinguish life if it were to increase or to continue, but the moment the patient stands still all this uneasiness vanishes”.[1]
Three major coronary arteries provide the heart with oxygenated blood, the right coronary artery (RCA), the left coronary artery (LCA) and the circumflex artery (Cx). When the coronary arteries are affected by atherosclerosis and the lumen of the coronary arteries narrows, the heart receives less oxygenated blood and becomes hypoxic, which results in angina pectoris.
Complete history and physical examination are essential to determine angina pectoris as diagnosis and to exclude other causes of chest pain, such as aorta dissection, arrhythmias, pulmonary embolism, pneumonia, heartburn, hyperventilation or musculoskeletal problems.[2]
History
Patients often experience angina pectoris as if a elephant stands on their chest. Because the heart itself has very few nerves the pain can be sensible elsewhere in the upper body, mainly arms, jaw and/or back.[3] Some patients only complain about stomach ache so the presentation can be very a specific.[4],[5]
Angina pectoris however has some characteristics that can help to differentiate between other causes of (chest) pain. Angina pectoris is gradual in onset and offset, with the intensity increasing and decreasing over several minutes. The pain is constant and does not change with respiration or position. If patients had angina pectoris before they will recognize the pain immediately.[6]
Angina pectoris usually occurs during exercise when the demand for oxygenated blood increases. Coronary arteries with a narrowed lumen can not meet the demand of oxygenated blood during exercise. As soon as the exercise is aborted angina pectoris decreases. This is called stable angina pectoris.
Unstable angina pectoris means angina pectoris at rest which consists less than two months. Over time the angina pectoris develops to more often, severe and prolonged, so that symptoms are to occur at less and less effort than before.[7]
Stable angina pectoris responds to nitro-glycerine spray, unstable angina pectoris does not. Nitro-glycerine spray is a venodilator which reduces venous return to the heart and therefore decreases the workload and therefore oxygen demand. It also vasodilates the coronary arteries and increases coronary blood flow.[8]
Nitro-glycerine is however not specific for angina pectoris, a similar response may be seen with oesophageal spasm or other gastrointestinal problems because nitro-glycerine also relaxes smooth muscle.[9]
During angina pectoris so called vegetative symptoms can occur, this includes sweating, nausea, paleface, anxiety and agitation. The idea is that the vegetative nerve system is more active in a reaction to stress.[10]
Physical Examination
Oxygen deficiency of the heart leads to ischemia, ischemia and the discomfort the patient experiences lead to sympathetic activation of the nervous system. This is detectable during physical examination by an increase in heart rate and elevation in blood pressure. Ischemia can also cause a temporarily impairment in myocardial function, on auscultation you could hear a paradoxically split second heart sound, a third or fourth heart sound and a mitral regurgitation murmur. All these findings however disappear with resolution of the ischemia. Up to date: Pathophysiology and clinical presentation of ischemic chest pain, geen bronvermelding.
ECG
The electrocardiogram (ECG) is an easy and important tool to differentiate between myocardial ischemia and infarction. Patients with unstable angina pectoris will show abnormalities on the ECG at rest, in particular ST depression. Patients with stable angina pectoris are likely to have a completely normal ECG at rest, exercise ECG testing will be necessary to show any abnormalities.[11] During exercise ECG testing an ECG is made during cycling on a home trainer or walking on a treadmill. While exercising the oxygen demand of the heart increases, if the narrowed coronary arteries are unable to supply enough oxygenated blood, the patient develops pain on the chest and the ECG will show abnormalities.[12]
Additional Research
If the ECG made during exercise testing does not show any abnormalities angina pectoris becomes very unlikely. If the ECG does show abnormalities during exercise testing additional research needs to be done.[13] Depending on the hospital one of the below standing research will be done.
- Exercise echocardiography means that an echocardiography is made directly after exercise. The poorly perfused parts of the heart will show less activity.[14]
- Myocardium Perfusion Scintigraphy (MPS) is able to show the perfusion of the heart during exercise and at rest.[15]
- MRI can be done with vasodilatory dobutamine or stimulating adenosine to assess how the heart behaves during exercise.[16]
The findings on stress testing can be used to determine the choice between medical therapy and revascularization in patients with stable angina. Coronary angiography is recommended based upon symptoms, left ventricular function, and estimated risk by stress testing.[17]
Table 1
Coronary Angiography
In patients with unstable angina pectoris early coronary angiography possibly followed by revascularization is usually performed within 4 to 24 hours of admission in the hospital. In most clinical trials this strategy has shown a reduction in the incidence of death or nonfatal myocardial infraction.[18]
A CAG is an X ray examination of the coronary arteries, a catheter is inserted into the femoral artery or into the radial artery. The tip of the catheter is positioned at the beginning of the coronary arteries and contrast fluid is injected. Contrast is visible by X ray and the images that are obtained are called angiograms.
On an angiogram stenoses will be visible, if the stenosis is significant coronary intervention will take place. Ideally this happens immediately following the CAG but not all hospitals that are entitled to carry out CAG are qualified to perform percutaneous coronary intervention (PCI).
Treatment
Medication
In patients with stable angina pectoris percutaneous coronary intervention does not offer any benefit in terms of death, myocardial infarction, or the need for subsequent revascularization compared with conservative medical treatment.[19]
Initial treatment of stable angina pectoris therefore focuses on medication to keep the workload of the heart as low as possible. β blockers lower heart rate and blood pressure, this decreases the oxygen demand of the heart.[20] Nitrates dilatate the coronary arteries so the heart receives more oxygenated blood.[21] Anticoagulants (aspirin) to reduce the risk of development of a thrombus in the coronary arteries.[22]
Apart from starting medication the patient needs to minimize any present risk factors like smoking, overweight and drinking alcohol. See chronic coronary diseases.
Percutaneous Coronary Intervention
The procedure of PCI is similar to a CAG, except this time a catheter with an inflatable balloon will be brought at the site of the stenosis. Inflation of the balloon within the coronary artery will crush the atherosclerosis and eliminate the stenosis. To prevent that the effect of the balloon is only temporarily a stent is often positioned at the site of the stenosis.
Coronary Artery Bypass Graft
There are circumstances in which CABG should be performed.
| Class of recommendations | Definition |
|---|---|
| Class I | Evidence and/or general agreement that a given treatment or procedure is beneficial, useful, effective. |
| Class II | Conflicting evidence and/or a divergence of opinion about the usefulness/efficacy of the given treatment or procedure.
|
| Class III | Evidence or general agreement that the given treatment or procedure is not usefull effective, and in some cases may be harmful. |
| Class I - There is evidence and/or general agreement that CABG should be performed in patients with STEMI in the following settings. | |
CABG does not eliminate the stenosis like PCI does. Using the internal thoracic arteries or the saphenous veins from the legs a bypass is made around the stenosis. The bypass originates from the aorta and terminates directly after the stenosis. Thereby restoring the blood supply to the ramifications.
Myocardial Infarction
In 2006 425.425 people died from a heart attack, 1.255.000 new and recurrent coronary attacks took place, about 34% died, 17.600.000 victims of angina, heart attack and other forms of coronary heart disease are still living.
These numbers only account for the United States.
Pathofysiology
A heart attack or myocardial infarction (MI) is an acute presentation of a process that has been going on much longer. The process responsible is atherosclerosis. Atherosclerosis is a chronic disease of the arteries in which artery walls thicken by deposition of fatty materials such as cholesterol. The result over decades are plaques, which can narrow the lumen of the arteries significantly and progressively causing symptoms as angina pectoris. Plaques can also suddenly rupture, trigger a cascade which results in a thrombus and thereby cause myocardial infarction.[23]
History
Classic presentation of a myocardial infarction is acute chest pain which lasts longer than a few minutes. PMID 16304077 The pain does not decrease at rest and is only temporarily relieved with nitroglycerin. Common accompanying symptoms are radiating pain to shoulder, arm, back and/or jaw. PMID 10099685 Shortness of breath can occur, as well as sweating, fainting, nausea and vomiting, so called vegetative symptoms. Some patients not really complain about chest pain but more about abdominal pain so as with angina pectoris the presentation can be very a specific. PMID 10866870, PMID 10751787
It is important to complete the history with information about past history (prior history of ischemic events or vascular disease), risk factors for cardiovascular disease (o.a. smoking, hypertension, hyperlipidemia, obesity) and family history (direct family with myocardial infarction and/or sudden cardiac death).
Signs of heart failure such as orthopnea (not able to sleep without a pillow), progressive dyspnoea and oedematous ankles are indicative for the extent of the problem. PMID 15289388
A suspected myocardial infarction should be rapidly evaluated to initiate appropriate therapy.
Physical Examination
On physical examination evidence of systemic hypoperfusion can be found such as hypotension, tachycardia, impaired cognition, pale and ashen skin. PMID 15289388
If during auscultation pulmonary crackles are heard and pitting oedema of the ankles is seen heart failure is complicating the myocardial infarction.
History and physical examination are helpful to determine myocardial infarction as diagnosis and to exclude other causes of chest pain, such as angina pectoris, aorta dissection, arrhythmias, pulmonary embolism, pneumonia, heartburn, hyperventilation or musculoskeletal problems. PMID 15289388
References
- Davies SW. Clinical presentation and diagnosis of coronary artery disease: stable angina. Br Med Bull. 2001;59:17-27. DOI:10.1093/bmb/59.1.17 |
- Sampson JJ and Cheitlin MD. Pathophysiology and differential diagnosis of cardiac pain. Prog Cardiovasc Dis. 1971 May;13(6):507-31. DOI:10.1016/s0033-0620(71)80001-4 |
- Foreman RD. Mechanisms of cardiac pain. Annu Rev Physiol. 1999;61:143-67. DOI:10.1146/annurev.physiol.61.1.143 |
- Canto JG, Shlipak MG, Rogers WJ, Malmgren JA, Frederick PD, Lambrew CT, Ornato JP, Barron HV, and Kiefe CI. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000 Jun 28;283(24):3223-9. DOI:10.1001/jama.283.24.3223 |
- Pope JH, Ruthazer R, Beshansky JR, Griffith JL, and Selker HP. Clinical Features of Emergency Department Patients Presenting with Symptoms Suggestive of Acute Cardiac Ischemia: A Multicenter Study. J Thromb Thrombolysis. 1998 Jul;6(1):63-74. DOI:10.1023/A:1008876322599 |
- Constant J. The clinical diagnosis of nonanginal chest pain: the differentiation of angina from nonanginal chest pain by history. Clin Cardiol. 1983 Jan;6(1):11-6. DOI:10.1002/clc.4960060102 |
- Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, Chavey WE 2nd, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Wright RS, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura R, Ornato JP, Page RL, Riegel B, American College of Cardiology, American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction), American College of Emergency Physicians, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association of Cardiovascular and Pulmonary Rehabilitation, and Society for Academic Emergency Medicine. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007 Aug 14;50(7):e1-e157. DOI:10.1016/j.jacc.2007.02.013 |
- Abrams J. Hemodynamic effects of nitroglycerin and long-acting nitrates. Am Heart J. 1985 Jul;110(1 Pt 2):216-24.
- Henrikson CA, Howell EE, Bush DE, Miles JS, Meininger GR, Friedlander T, Bushnell AC, and Chandra-Strobos N. Chest pain relief by nitroglycerin does not predict active coronary artery disease. Ann Intern Med. 2003 Dec 16;139(12):979-86. DOI:10.7326/0003-4819-139-12-200312160-00007 |
- Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK, and American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation. 2004 Aug 3;110(5):588-636. DOI:10.1161/01.CIR.0000134791.68010.FA |
- Guidelines for cardiac exercise testing. ESC Working Group on Exercise Physiology, Physiopathology and Electrocardiography. Eur Heart J. 1993 Jul;14(7):969-88.
- Fox K, García MA, Ardissino D, Buszman P, Camici PG, Crea F, Daly C, de Backer G, Hjemdahl P, López-Sendón J, Morais J, Pepper J, Sechtem U, Simoons M, Thygesen K, and Grupo de trabajo de la sociedad europea de cardiologia sobre el manejo de la angina estable. [Guidelines on the management of stable angina pectoris. Executive summary]. Rev Esp Cardiol. 2006 Sep;59(9):919-70. DOI:10.1157/13092800 |
- Fox K, García MA, Ardissino D, Buszman P, Camici PG, Crea F, Daly C, de Backer G, Hjemdahl P, López-Sendón J, Morais J, Pepper J, Sechtem U, Simoons M, Thygesen K, and Grupo de trabajo de la sociedad europea de cardiologia sobre el manejo de la angina estable. [Guidelines on the management of stable angina pectoris. Executive summary]. Rev Esp Cardiol. 2006 Sep;59(9):919-70. DOI:10.1157/13092800 |
- Amanullah AM and Lindvall K. Predischarge exercise echocardiography in patients with unstable angina who respond to medical treatment. Clin Cardiol. 1992 Jun;15(6):417-23. DOI:10.1002/clc.4960150605 |
- Brown KA. Prognostic value of thallium-201 myocardial perfusion imaging in patients with unstable angina who respond to medical treatment. J Am Coll Cardiol. 1991 Apr;17(5):1053-7. DOI:10.1016/0735-1097(91)90829-x |
- Kwong RY, Schussheim AE, Rekhraj S, Aletras AH, Geller N, Davis J, Christian TF, Balaban RS, and Arai AE. Detecting acute coronary syndrome in the emergency department with cardiac magnetic resonance imaging. Circulation. 2003 Feb 4;107(4):531-7. DOI:10.1161/01.cir.0000047527.11221.29 |
- Fraker TD Jr, Fihn SD, 2002 Chronic Stable Angina Writing Committee, American College of Cardiology, American Heart Association, Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, Ferguson TB Jr, Gardin JM, O'Rourke RA, Williams SV, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura R, Page RL, Riegel B, Tarkington LG, and Yancy CW. 2007 chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. J Am Coll Cardiol. 2007 Dec 4;50(23):2264-74. DOI:10.1016/j.jacc.2007.08.002 |
- Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, Chavey WE 2nd, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Wright RS, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura R, Ornato JP, Page RL, Riegel B, American College of Cardiology, American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction), American College of Emergency Physicians, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association of Cardiovascular and Pulmonary Rehabilitation, and Society for Academic Emergency Medicine. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007 Aug 14;50(7):e1-e157. DOI:10.1016/j.jacc.2007.02.013 |
- Katritsis DG and Ioannidis JP. Percutaneous coronary intervention versus conservative therapy in nonacute coronary artery disease: a meta-analysis. Circulation. 2005 Jun 7;111(22):2906-12. DOI:10.1161/CIRCULATIONAHA.104.521864 |
- Fox K, Garcia MA, Ardissino D, Buszman P, Camici PG, Crea F, Daly C, De Backer G, Hjemdahl P, Lopez-Sendon J, Marco J, Morais J, Pepper J, Sechtem U, Simoons M, Thygesen K, Priori SG, Blanc JJ, Budaj A, Camm J, Dean V, Deckers J, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Tamargo J, Zamorano JL, Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology, and ESC Committee for Practice Guidelines (CPG). Guidelines on the management of stable angina pectoris: executive summary: The Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology. Eur Heart J. 2006 Jun;27(11):1341-81. DOI:10.1093/eurheartj/ehl001 |
- Abrams J. Hemodynamic effects of nitroglycerin and long-acting nitrates. Am Heart J. 1985 Jul;110(1 Pt 2):216-24.
- Hennekens CH, Dyken ML, and Fuster V. Aspirin as a therapeutic agent in cardiovascular disease: a statement for healthcare professionals from the American Heart Association. Circulation. 1997 Oct 21;96(8):2751-3. DOI:10.1161/01.cir.96.8.2751 |
- Davies MJ. Pathophysiology of acute coronary syndromes. Indian Heart J. 2000 Jul-Aug;52(4):473-9.